APC in the Dominican Republic FY16
Jump to sections on:
APC's goal is to contribute to a sustainable reduction in HIV transmission among key populations and to promote an improved quality of life for people living with HIV.
In the Dominican Republic (DR), APC serves populations with the highest HIV prevalence by expanding coverage and improving the quality of HIV-prevention, care, and support services.
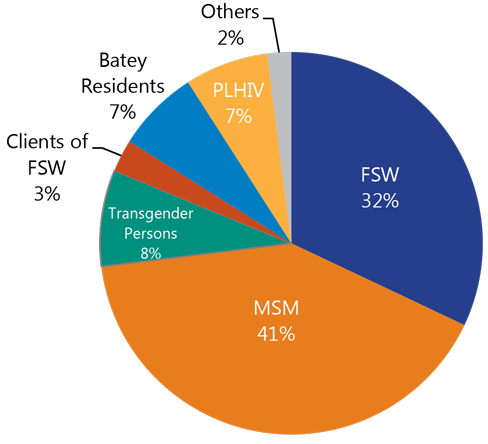
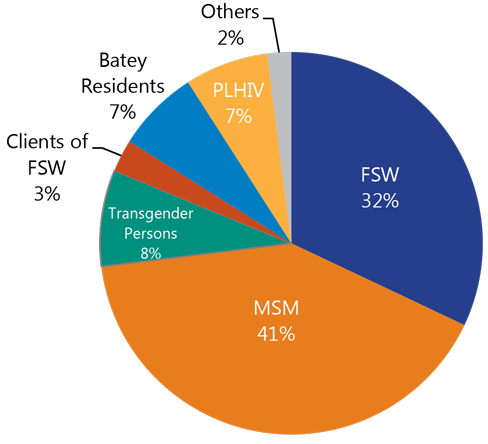
By partnering with local organizations, APC has been able to reach key populations–female sex workers, men who have sex with men, and transgender persons–as well as priority populations such as clients of sex workers and batey residents.
In 2016, APC has continued to build on the success of fiscal years 2014 and 2015 through technical assistance and support provided to 22 local organizations and public hospitals.
During the first semester of FY16 (October 1, 2015 through March 31, 2016), APC partners continue reaching members of key and priority populations with community-based HIV prevention.
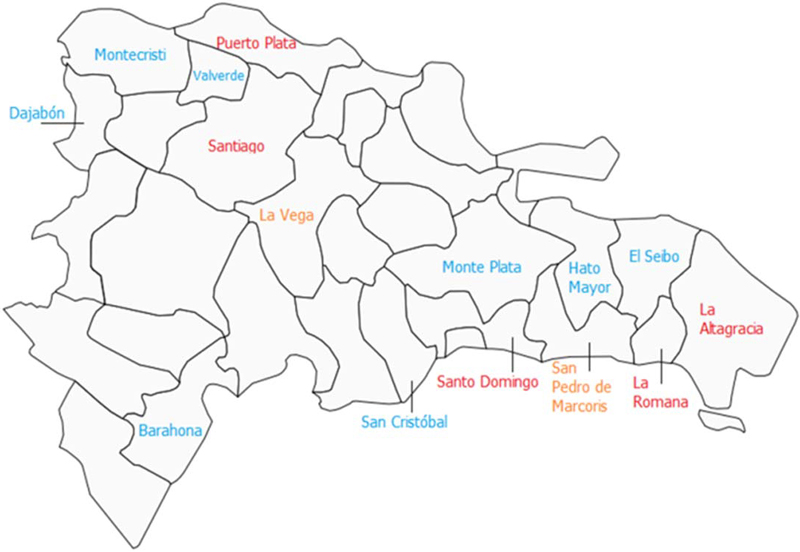
Provinces in the Dominican Republic in which APC worked during FY16
APC partners also accompanied key and priority populations to HIV testing and counseling HTC services, linked people who were diagnosed as HIV-positive to care, and improved the adherence of patients in antiretroviral therapy.
I was treated with respect by the doctor and other staff at the clinic, and the counselor helped talk me through my fears about getting an HIV test... When I received my results, we talked about what I needed to do to stay HIV-negative. I wanted to make sure my friends got the same information.
-Beneficiary from Clínica de Familia
Prevention
HIV Prevention
APC is committed to improving access to a comprehensive package of HIV and sexually transmitted infection (STI) prevention, treatment, community care, and support services for key and priority populations.
The package includes:
- information, education, and communication activities
- HIV testing and STI treatment services
- accompanied referrals to HTC services
- accompanied referrals to STI services
- provision of condoms and lubricants
- referral to HIV clinical care and treatment services.
For me, it was important that the person who contacted me assure me that the test is confidential and if the result was positive, COIN would provide me with ongoing care and support.
-Amalis, a sex worker who was introduced to HIV testing through the APC's grantee Center for Comprehensive Orientation and Investigation's (COIN in Spanish) mobile clinic.
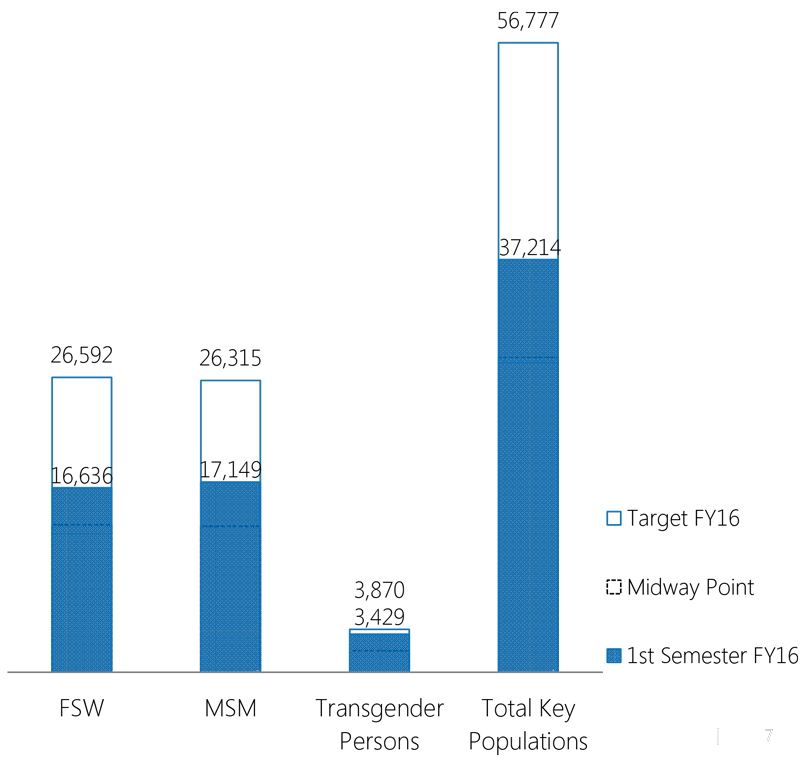
Key Populations Reached with HIV-Prevention Services
During the first semester of FY16, seven consortia consisting of 22 APC grantees and subgrantees organized prevention activities in 14 provinces, reaching 37,214 members of key populations.
Individuals from key population reached with standardized HIV-prevention interventions
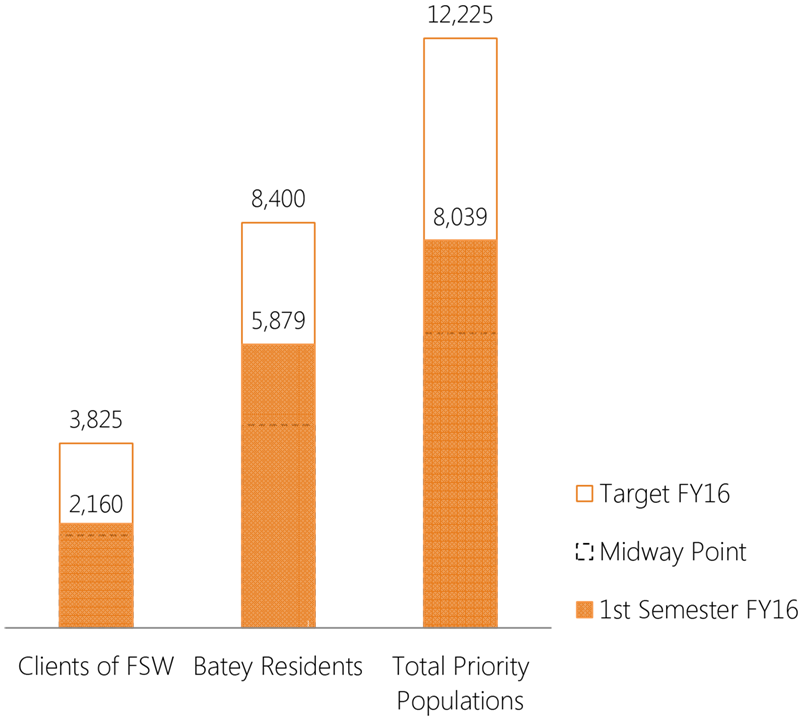
Priority Populations Reached with HIV-Prevention Services
APC partners reached 8,039 members of priority populations with evidence-based, minimum standard HIV-prevention interventions during the first semester of FY16.
Individuals from priority population reached with standardized HIV-prevention interventions
Linkages and Referrals
Referrals and counter-referrals to HIV testing and STI treatment services are essential components of APC prevention activities. The referral system ensures the timely diagnosis of HIV in key and priority populations, immediate entry to comprehensive care services at APC clinics and public sector hospitals, and access to treatment for STIs identified in these health centers. During the first semester of FY16, APC partners made 15,038 referrals to these services (64 percent of the FY16 target). The highest numbers of referrals were for HIV testing. Of all referrals, 97 percent were counter-referrals.
 |
 |
 |
 |
 |
| Referrals to services | HIV testing and STI treatment | Diagnosis of HIV in key and priority populations | Enrollment in comprehensive care services at APC clinics and public sector hospitals | Counter-referrals |
Distribution of Condoms and Lubricants
During the reporting period, APC distributed 755,648 condoms and 673,968 lubricants to key and priority populations as part of the minimum prevention package. PLHIV also had access to condoms and lubricants as part of the positive prevention package. These activities were conducted according to USAID criteria for distribution of donated condoms.
755,648 condoms
673,968 lubricants
HIV Counseling and Testing
Knowing one's HIV status is essential to preventing the spread of HIV and accessing counseling and medical care.
HIV testing and counseling (HTC) is the first link in the 90-90-90 PEPFAR strategy, as it allows early entry of people with HIV-positive diagnoses to comprehensive care and antiretroviral treatment.
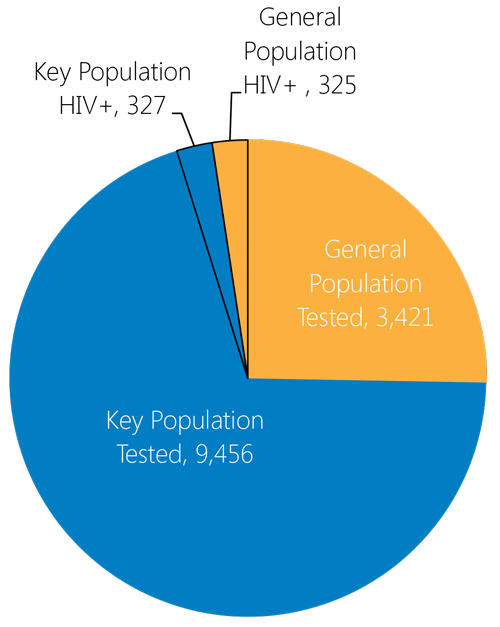
People Reached with HTC Services
During the first semester of FY16, APC offered direct HTC services (with pre- and post-counseling), to 12,877 people. Of this total, 9,456 were key populations and 3,421 were members of the general population. Of the 12,877 reached with HTC services, 652 tested positive (327 key population and 325 general population individuals), for a yield of 5.1 percent. People who received HTC services were reached through direct services from APC partners in mobile clinics and community events.
People reached with HTC services directly by APC partners
Care and Support for People Living with HIV
Clinical care services and community support are essential for people diagnosed with HIV.
A variety of approaches–enrollment and retention in service, ensuring early access to ART, etc.–help PLHIV have a better quality of life. These services are part of a continuum of care offered from the time of initial HIV diagnosis, prior to and during ART, to end-of-life care. APC-supported care and support includes clinical, psychological, social, spiritual, and prevention services designed to increase retention in care, maximize functional ability, and minimize morbidity.
Ever since I came to IDEV six months ago, everyone has treated me well. I remember that during my first appointment, they asked me the first thing that came to mind when I heard the term HIV and AIDS, and I said, 'to try to overcome this problem', but If I were asked the same question today, I would answer, 'HIV is not a death sentence, but a chance to live.'
- Jose Julio, IDEV patient
Community-based Services
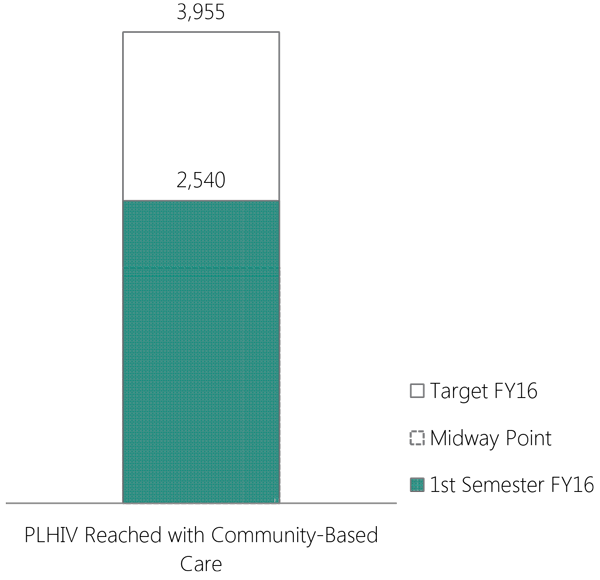
APC community promoters provided a package of interventions to PLHIV that included clinical care, psychological and social support, and financial assistance to cover transportation costs.
2,540 PLHIV (64 percent of target) were reached through community health promotors who offer services in 14 provinces. These services focused on retention, recovery of those considered lost to follow-up, and adherence to treatment. This was achieved through close coordination between APC-supported clinics that offer health services and the HIV comprehensive care clinics at public hospitals. In addition, during this reporting period, 529 of 2,196 PLVIH who had dropped out of care were recovered at 14 health centers. This represented recovery of 24 percent of the dropouts recorded at the beginning of the year.
Number of PLHIV reached with community-based care
Direct Clinic-Based Services
Clinical services include psychological counseling, clinical evaluation, CD4 and viral load testing, ARV delivery (per the National Guidelines for HIV/AIDS Care), counseling for treatment adherence, positive prevention, screening for tuberculosis, STI treatment, and family planning services.
Antiretroviral therapy (ART)
The number of patients on ART enrolled at the seven APC supported clinics represent 19 percent of the total PLHIV on ART in all 76 comprehensive care clinics (SAIs in Spanish) in the country.
Total patients on ART in all 76 SAIs in the DR as of March 2016
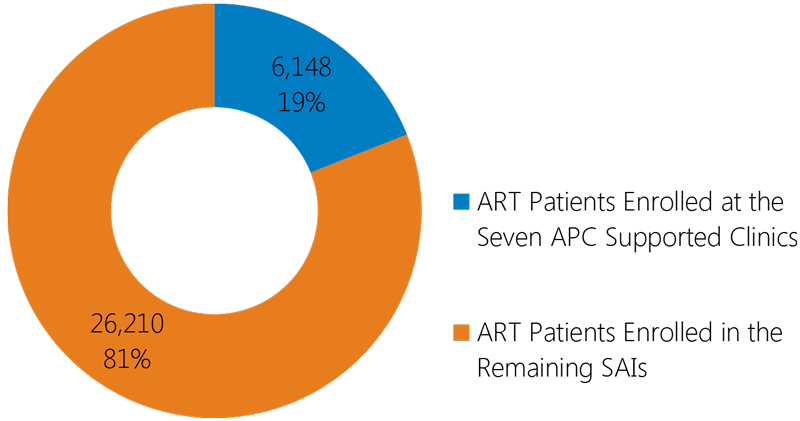
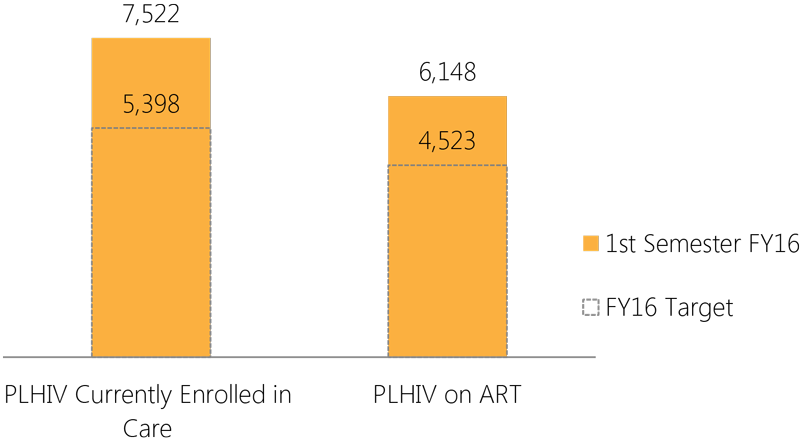
In the first half of FY16, October 2015–March 2016, the Application Form for Social Policy Programs (FAPPS in Spanish) reported 7,522 PLHIV currently enrolled in care in the seven APC-supported clinics, surpassing the FY16 annual target of 5,398 by 139 percent. In addition, 6,148 of these patients are on ART, surpassing the FY16 annual target of 4,523 by 136 percent.
PLHIV receiving direct clinical services in the seven APC-supported clinics
Indirect Clinic-Based Services
During the first semester of FY16, APC through its partners referred and/or accompanied PLHIV to HTC services in public sector hospitals and clinics. Some were newly diagnosed at HTC community events. A total of 377 PLHIV were enrolled in HIV clinical care at 10 public hospitals and one nongovernmental organization (NGO) clinic.
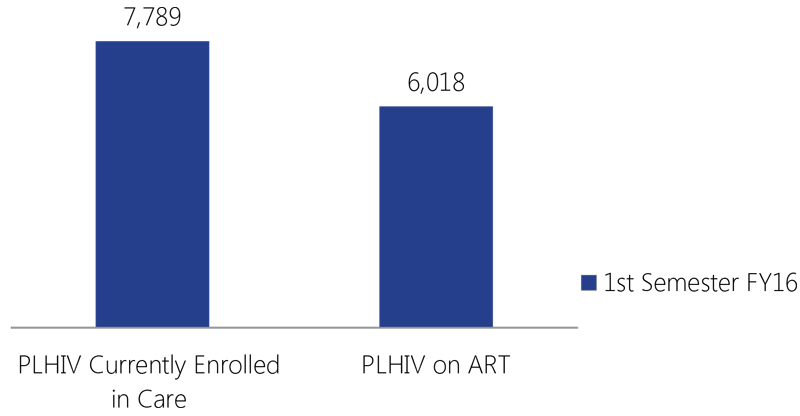
The FAPPS reported 7,789 PLHIV currently enrolled in care in the 10 SAIs that receive technical assistance from APC grantees. These SAIs reported 6,018 patients on ART, representing 77 percent of the total number of patients enrolled in care.
PLHIV who receive services at the 10 SAIs that receive TA from APC grantees
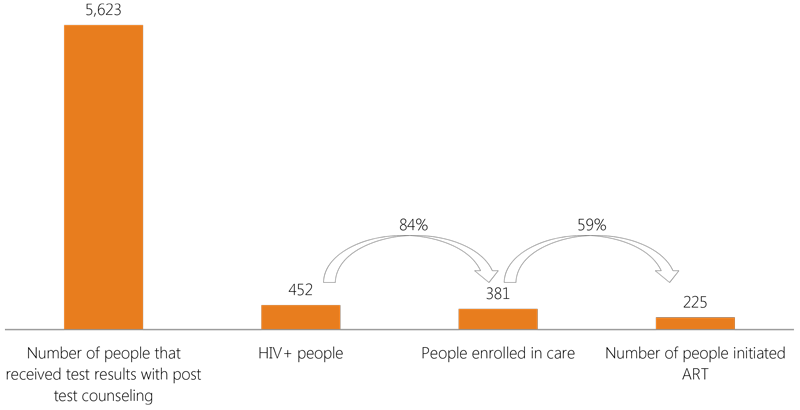
HIV Treatment Cascade at Clinical Sites
The HIV treatment cascade is an essential resource for monitoring the number of people who receive HIV services at clinical sites.
The cascade illustrates the progress of a person who is receiving HIV services through every stage of treatment before s/he achieves viral suppression.
APC uses the HIV treatment cascade to identify opportunities to ensure that APC reaches the PEPFAR 90-90-90 goals.
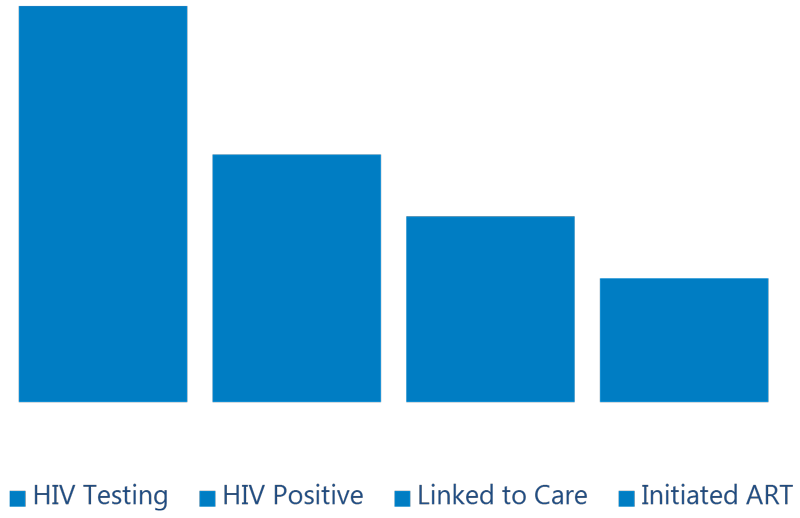
The treatment cascade begins with the HIV test and the delivery of the results. The next stage is linking people who are positive to care, which includes clinical evaluation, periodic CD4 and viral load measurements, and other services. Once a patient is enrolled in care, the effectiveness of the treatment depends on the patient remaining in care. Adherence to ART is closely associated with viral suppression; if an ART patient adheres to treatment (≥95 percent), the probability of achieving viral suppression will be higher.
HIV treatment cascade of people reached with comprehensive care through
direct and indirect services during the first semester of FY16
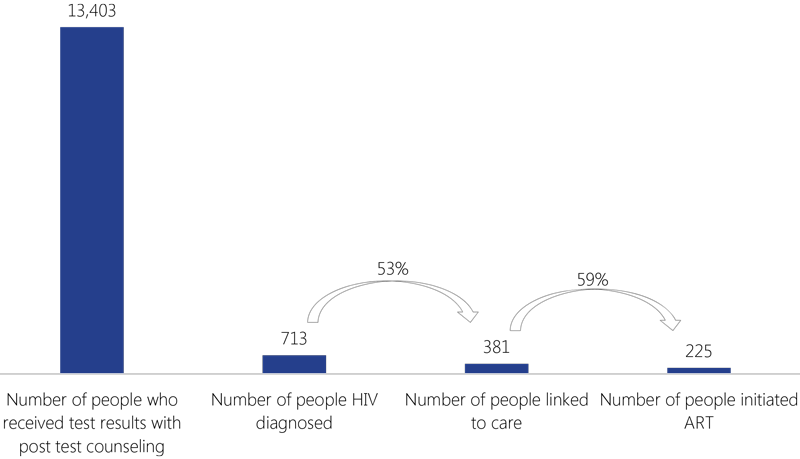
HIV treatment cascade of people reached with comprehensive care through
clinics supported by APC during the first semester of FY16
Adherence to Treatment
Adherence to treatment helps prevent drug resistance and helps patients reach an undetectable viral load, which improves quality of life and lowers the probability of infecting others.
APC began studying adherence of patients on ART at APC-supported clinics in 2014. Adherence was measured through a review of ARV dispensing records during similar time periods to determine if patients were picking up their refills of ARV drugs on time.
The advantage of this type of measurement is that adherence can be assessed using existing data on dispensation of ARV drugs. The disadvantage is that this measurement may overestimate adherence since it does not assess actual adherence of patients taking their ARV drugs as prescribed, and may underestimate adherence if ARV drug dispensation is not well-documented.
I was afraid of getting tested... I didn't even wait for the results. It was not until a health promoter went to my house to talk to me in private about the importance of knowing my status that I decided to face the outcome.
- Kissairys, a female sex worker who was recently diagnosed with HIV.
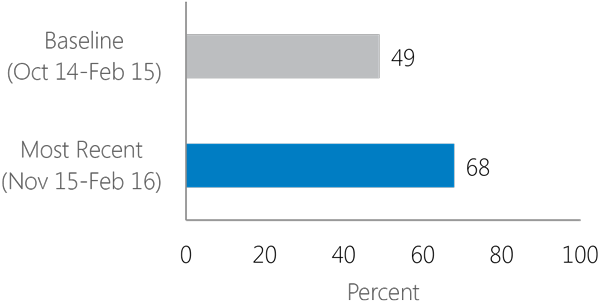
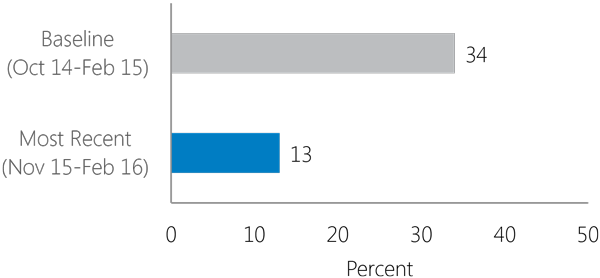
Adherence to ART
Adherence to ART measurements using dispensing records during October 2014–February 2015 and November 2015–February 2016. Over these two periods, adherence to ART increased with a concomitant decrease in non-adherence.
These improvements are due partly to improvements in ART adherence (as measured by ARV dispensing records) and partly to improvements in documentation of ARV dispensation.
Increasing adherence to treatment (adherence equal or higher than 95%)
Decreasing non-adherence to treatment (less than 80% adherence)
Viral Load
Viral load (VL) tests provide important information about the health status of HIV-positive patients. If a patient is on ART, viral load tests can also indicate the effectiveness of the treatment.
Percent of ART patients with viral load result during the past 12 months
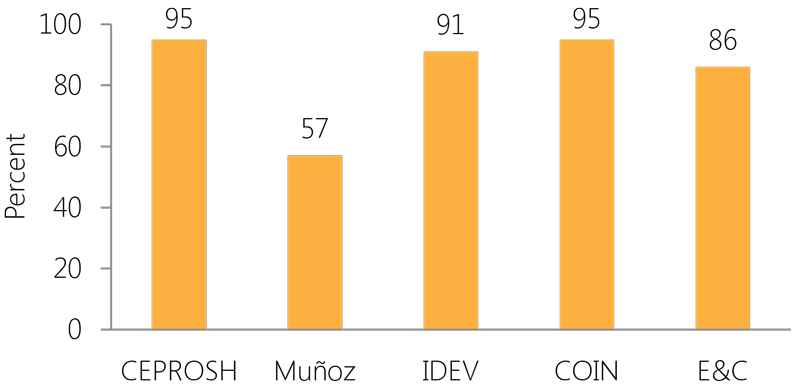
Although it is recommended that VL be monitored every 6-12 months, VL testing is very limited in low-resource settings. During the most recent measurements of ART adherence, APC reviewed the patients' VL test results. While obtaining VL results has long been problematic for many facilities, APC is proud to show that an average 85 percent of patients on ART at APC-funded clinics have received their viral load results.
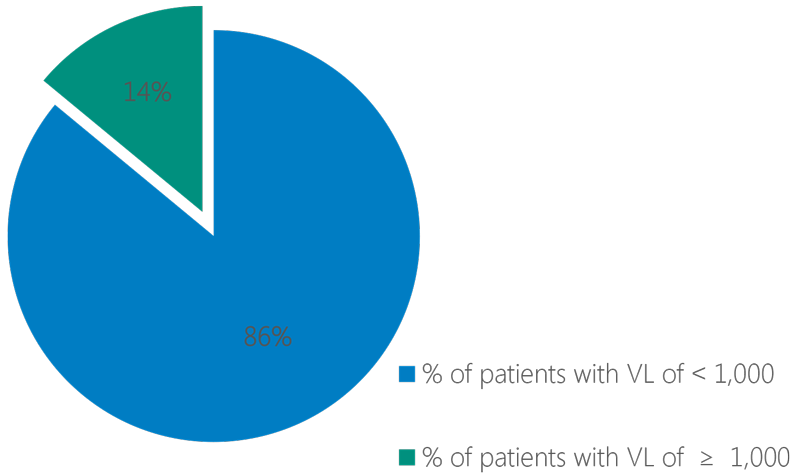
ART Adherence and Viral Load
Comparing viral load results and ART adherence (as measured by ARV dispensing records) in patients who had been on ART for at least six months and who had a VL result during the 12 months prior to the assessment. 86 percent of patients have VL < 1,000 copies per milliliter vs. 14 percent of patients who have VL > 1,000 copies.
Not all patients who adhere to ART as measured by ARV dispensation have a VL <1,000. Patients who have good adherence may have problems actually taking their ARVs as prescribed. In addition, some patients in this sample had a viral load test prior to initiation of ART.
Patients who have an adherence of ≥95% with a viral load of <1,000 copies per ml
Improving Quality of Services
APC and its partners guide key and priority populations through the HIV treatment cascade while improving the quality of services.
During the first semester of FY16, APC continued advocating for human rights and the implementation of anti-discrimination policies in several NGO clinics and public hospitals.
As part of improving the quality of services, APC also surveyed transgender people to identify barriers that prevent this population's access to HIV services.
We developed a satisfaction survey to be filled out by patients who receive HIV services in all 14 hospitals throughout the region. We also implemented a tool developed by an APC international technical advisor to measure adherence to HIV treatment.
- Dr. Elsa Valdez, manager of the Region V Health Service (SRS)
Improving Pharmacy Storage and Dispensing Practices
When APC assessed the quality of clinical services in 2015, it identified the need to strengthen storage and dispensing practices in the clinic pharmacies. APC asked MSH's USAID-funded Systems for Improved Access to Pharmaceuticals and Services (SIAPS) project for support to conduct a training workshop on pharmacy storage and dispensing practices.
Outcomes of the workshop:
 |
 |
 |
| All APC-supported clinics now have hydrogen thermometers to measure the temperature and humidity of stock rooms. | Most clinics also made changes in the physical space and are implementing dispensation through prescription so that patients receive their medications at the pharmacy. | APC also helped the clinics to develop and implement quality improvement plans. |
Health Services for the Transgender Population
APC conducted an assessment of the health needs of transgender persons with the goal of using the results to improve the quality of services offered to this population in priority provinces of the DR.
Members of the transgender population were trained to conduct a survey throughout Santo Domingo, San Pedro de Macorís, La Romana, La Altagracia, Espaillat, La Vega, Santiago, Puerto Plata, and Samaná. They conducted 299 interviews, and four focus groups were organized with transgender women, and two with transgender men.

Human Rights, Stigma, and Discrimination/Gender-Based Violence

APC addressed stigma and discrimination, reduced gender-based violence, and promoted human rights through 15 partner organizations that have community programs, seven clinics, and support 10 public-sector hospitals.
During the first semester of FY16, APC-
- established a working group to address stigma and discrimination with APC partner organizations
- trained 12 staff members of APC partner organizations in the documentation and management of stigma and discrimination cases
- trained 240 clinical services providers to address stigma and discrimination
- designed anti-discrimination policies to support clinical and community services in 14 provinces
- implemented a mechanism between hospital authorities and organizations representing key populations to coordinate anti-discrimination actions at seven public health facilities.
