The Community-based Health System Model Series briefs identify and discuss critical health system inputs and processes that have contributed to the implementation and expansion of community-based service delivery in different countries. Countries were selected for their geographic diversity, type of service delivery model, and programmatic scale-up. This brief reviews Malawi’s community health model to inform future policy, program design, and implementation in other countries. Read briefs on Nepal | Senegal

Photo: Feed the Children/Wezzie Grace Kenan
Health Situation in Malawi
Over the past three decades, Malawi has made great strides in improving key health indicators. Maternal mortality declined by one-third, from 957 to 634 deaths per 100,000 live births between 1990 and 2015.1 The percentage of births delivered by a skilled attendant increased from 54.2 percent in 2000 to 89.8 percent in 2015.2,3
Over the same period, stunting in children under five years of age declined from about half to just over a third, and the percentage of children sleeping under a mosquito net increased from 7.6 to 44.7 percent.2,3 Most notably, Malawi reached Millennium Development Goal 4, achieving a 72 percent reduction in child mortality between 1990 and 2015, from 242 deaths per 1,000 live births to just 64.4
In the last 15 years, modern contraceptive use among married women has more than doubled, from 26.1 percent in 2000 to 58.1 percent in 2015, one of the highest rates in all of sub-Saharan Africa.2,3 This progress has been accompanied by a decline in the total fertility rate from 5.7 in 2010 to 4.4 in 2015.3,5 Table 1 indicates key health statistics in Malawi.
Table 1. Current Health Statistics in Malawia
| Total populationb | 17.2 M |
| Rural populationb | 84% |
| Total fertility rate | 4.4 |
| Contraceptive prevalence rate (modern methods) | 58.1% |
| Maternal mortality ratio (per 100,000 live births)c | 634 |
| Neonatal mortality rate (per 1,000 live births) | 27 |
| Infant mortality rate (per 1,000 live births) | 42 |
| Under-five mortality rate (per 1,000 live births) | 64 |
| Percentage of births delivered by a skilled provider | 89.8% |
| Percentage of children moderately or severely stunted | 37.1% |
| Percentage of households with an improved source of drinking water | 87.2% |
| Percentage of women reporting distance to a health facility as a problem in accessing health cared | 57% |
| Adult HIV prevalencee | 9.1% |
| Total expenditure on health per capita (current US$)f | $29 |
a Data is from the Malawi Demographic and Health Survey, 2015-16 Key Indicators Report,3 unless otherwise noted.
b Population Reference Bureau (PRB). 2016. 2016 World Population Data Sheet. Washington, DC: PRB.
c World Health Organization. 2015. Trends in Maternal Mortality 1990 to 2015: estimates by WHO, UNICEF, UNFPA, World Bank Group and the United States Population Division. Geneva: World Health Organization.
d National Statistical Office (NSO) and ICF Macro. 2011. Malawi Demographic and Health Survey 2010. Zomba, Malawi, and Calverton, Maryland, USA: NSO and ICF Macro.
e UNAIDS. 2015. “HIV and AIDS estimates” (2015).
f World Bank Data Bank 2010-2014. “Health expenditure per capita (current US$).”
These successes may be linked to several factors. Adopting and scaling up evidence-based interventions, such as community-based distribution of family planning (FP) and integrated community case management (iCCM) for childhood illness, enabled more equitable access to essential health services. Also, expanded support to community health providers has filled gaps in health service delivery.
Despite Malawi’s health achievements, there is room for progress. Seventy percent of all child deaths are due to preventable causes, including malaria, diarrhea, pneumonia, anemia, and malnutrition.6 The country’s neonatal mortality rate is among the highest in the world, with an estimated 27 deaths per 1,000 live births.3 Still, the country has laid important groundwork for reaching new national and global health targets, such as the Sustainable Development Goals and Family Planning 2020 commitments.
Figure 1. Under-five, Infant, and Neonatal Mortality in Malawi, 2000-2015*

Figure 2. Modern Contraceptive Use in Married Women, Rural and Urban
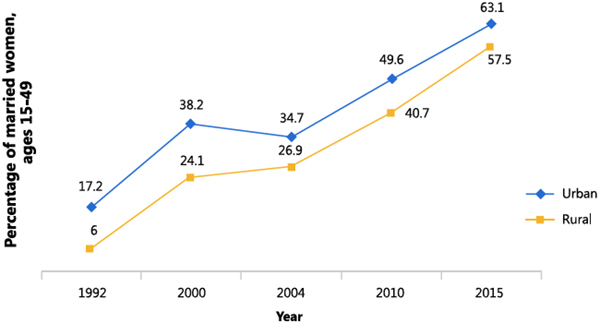
*Data are from the Malawi Demographic and Health Surveys, 1992-2016
Malawi’s Health System Structure: Community Health Providers Help Improve Coverage
Malawi’s Ministry of Health (MOH) determines the direction of the country’s health and development sector through national-level policy guidance. In 1998, the Government of Malawi (GOM) designated greater political and administrative authority to the district level, with district councils and the district health office (DHO) overseeing planning, implementation, and coordination of health activities, including at the community level, often with the support of nongovernmental organizations, other private sector organizations, and civil society. The health system comprises primary, secondary, and tertiary levels of care linked through a referral system. Most Malawians access health services at the primary level. Both the public and private sectors play crucial roles in delivering health services. Figure 3 captures Malawi’s health system structure.
Figure 3. Malawi’s Public Health System 10-13
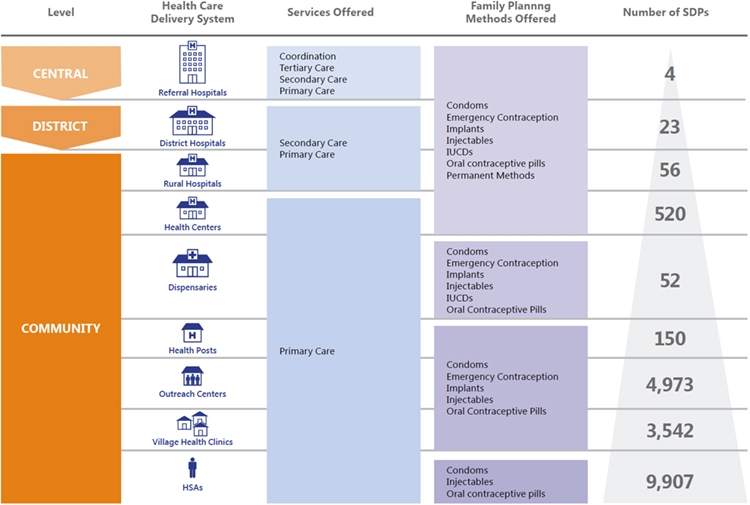
Today, Malawi has approximately 10,000 health surveillance agents (HSAs) deployed in communities across the country, comprising one-third of the health workforce.7 HSAs have been active since the 1950s when they provided immunizations.8 In 1998, HSAs were integrated into the formal health system.7 Each HSA is linked to a primary-level health facility but also delivers a range of services in communities in accordance with the country’s Essential Health Package (EHP). These services include information on hygiene and sanitation; immunizations; growth monitoring; antenatal and postnatal care education; nutrition counseling; FP; disease surveillance; HIV testing and counseling; iCCM; and other basic curative health services.9
In addition to the HSAs, other community health cadres, listed in Table 2 on page 4, conduct health promotion and provide services across many health areas. Over the years, Malawi has integrated these different community health provider cadres into its health system and substantially expanded the array of services they provide to increase access and improve health outcomes.
Key Community Health System Inputs: Policy to Service Delivery
Policymakers and program planners determine community health providers’ practices and procedures based on the local context, taking into consideration the burden of disease, community priorities, available resources, and capacity. Table 2 captures this information, with a focus on HSAs.
Table 2. Key Inputs in Malawi’s Community Health Programs
| INPUT | MALAWI'S COMMUNITY HEALTH PROGRAM |
|---|---|
| Supportive policy | A vast number of policies and strategies guide community health, including: - Essential Health Package, 2004 (updated in 2010) - Health Sector Strategic Plan, 2011–2016 - National Health Surveillance Assistant Programme of Malawi, 2013 |
| Selection | The GOM recruits HSAs. Candidates must speak English and the local language; be 19 years of age or older; and have a minimum of a Malawi School Certificate of Education. Selection processes and criteria vary for other cadres, but often they are selected by the community they serve. |
| Supervision and management | Health facility staff (senior HSAs, environmental health officers, community health nurses) conduct quarterly supervision visits for HSAs, who supervise other community-level cadres. |
| Commodities and materials | HSAs may provide iCCM drugs, FP products (condoms, pills, and injectables), growth monitoring supplies, and HIV and AIDS testing and care supplies. They also use educational materials. Other cadres provide commodities and supplies specific to their health areas. |
| Training | HSAs receive a 12-week training (8 weeks classroom-based and 4 weeks practical) followed by a final exam. HSAs who implement iCCM undergo another 6-day training. Refresher trainings are need-based, not regular. Training for other cadres varies. |
| Incentives | HSAs receive salaries (approximately US$63 per month), per diems, and non-financial incentives (uniforms, t-shirts, bags, public recognition). Other cadres receive incentives based on the programs that support them. |
| Referrals | Other community health provider cadres refer clients to HSAs for services they do not provide. HSAs refer patients to a the nearest health facility for care beyond their scope. |
| Health promotion | All community health providers conduct health promotion related to their areas of expertise, at community group meetings, facilities, and door-to-door. |
| Monitoring and reporting | HSAs collect routine data and compile them into reports, incorporating data from the cadres they supervise. They submit reports to the facility level to be consolidated, forwarded to the district, and entered into the health management information system. Data flow back down the health system through reports and meetings. |
| Scope of practice | - HSAs provide basic preventive and curative primary health care services, supervise other cadres, and maintain village health registers. - Community-based distribution agents (CBDAs) conduct FP counseling and provide condoms and oral contraceptive pills. - Community home-based care volunteers manage simple ailments (cough, fever, diarrhea, and other symptoms of common HIV opportunistic infections) and provide psychosocial support and nutrition counseling to people living with HIV. - Community leaders for action on nutrition mobilize and train community caregivers, such as parents, on implementation and monitoring of nutrition-related activities. - Natural leaders mobilize communities and lead community-led total sanitation efforts to help communities become open defecation-free. - Village health committees conduct community mobilization, monitor and report health issues, and educate about healthy behaviors. - Water point committees oversee the operation and management of community water points. |
Key Strategies for Strengthening and Scaling up Malawi’s Community Health Programs
1. Implementing responsive and forward-thinking policies and strategies that scale up maternal and child health interventions
Over time, the GOM has developed policies and strategies that respond to the needs of the population and provide critical direction for community health programs. In the past 20 years, supportive policies have directed the scale-up of community-based distribution of FP and iCCM.
Family Planning Policies
In 1994, the GOM developed the National Population Policy, which adopted a holistic approach to curtailing population growth and improving maternal and child health outcomes by increasing contraceptive use, promoting safe motherhood, boosting economic development, and reducing unemployment.14 Around the same time, the country updated its national FP guidance to provide an enabling environment for accessing contraception.15 Most notably, women no longer needed the consent of their husbands to initiate FP. These advances helped create the conditions in which contraceptive prevalence tripled from 7.4 percent in 1992 to 26.1 percent in 2000.2,16
The 2002 Reproductive Health Programme accelerated implementation of community FP initiatives, such as piloting community-based distribution of pills and condoms, and health promotion and awareness-raising.15 Malawi’s 2004 EHP, which included FP services, stipulated that all people could receive essential health products and services for free, thereby reducing barriers to access.17
In 2000, the injectable contraceptive use rate among married women in Malawi was approximately 16 percent.2 In 2008, Malawi became one of the first sub-Saharan African countries to allow community-based provision of injectable contraceptives by task-shifting to HSAs.18 Since then, the country has piloted and scaled up the intervention, and injectable use has surged, reaching 30 percent in 2015 and is now the method of choice for over half of women using FP.3 As a result, a 2010 assessment found that fewer women had to come to health centers for FP, which reduced the workload of facility-based workers. Many Community-based distribution agents (CBDAs), who provide only pills and condoms, also noted a lighter workload because of the availability of injectables in communities by HSAs. In 2015, the MOH and partners began piloting the feasibility of community-based administration of Sayana® Press, a small and easy-to-use injectable contraceptive, by HSAs as well as through self-injection by users. Results are expected mid-2017.19
In response to the soaring uptake of injectables, the GOM has included piloting CBDA administration of injectables in the Malawi Costed Implementation Plan for Family Planning, 2016–2020.20 Additionally, the plan aims to pilot HSA provision of implants, an FP method growing in popularity in Malawi, with use among married women increasing from 1.3 percent in 2010 to 11.5 percent in 2015.3,5
Integrated Management of Childhood Illness Policies
Malawi has also led the way in improving health outcomes through political leadership and supportive policies to guide integrated management of childhood illness (IMCI) interventions. In the late 1990s, the GOM developed and implemented an IMCI strategy that focused on curative services in health facilities, and launched a presidential initiative allowing HSAs to provide basic care for minor ailments, setting a precedent for treatment within community programs.21
In 2007, the GOM recognized that facility-based IMCI interventions were not reaching those most in need and developed a new IMCI strategy to scale up key community-based interventions in child health, making Malawi an early adopter of iCCM.21 The policy led to the introduction of high-impact interventions, including supplying oral rehydration salts and zinc for diarrhea management and insecticide-treated nets (ITNs) to protect children and women from malaria. It also placed some HSAs in village clinics, which clients appreciated. Findings from a 2015 study showed that caregivers preferred going to village clinics because they were nearby; viewed HSAs as reachable, trustworthy, and respectful; and medicines were frequently in stock.12
iCCM introduction came at an opportune time, coinciding with a doubling of Malawi’s HSA workforce from 5,000 to 10,000.22 The country was thus able to leverage the HSAs to implement iCCM, given their experience delivering services in communities and their wide national coverage. HSAs began implementing iCCM in 2009 after the GOM and World Health Organization collaborated to adapt IMCI algorithms for community-level use and incorporated them into an HSA training manual.21
By 2014, there were 9,907 HSAs in the country, 4,572 of whom were trained in iCCM.21 A recent study has shown that while HSAs still have room for improvement in identifying danger signs and treating illness among children, the quality of care they provide is similar to that of facility-based workers.23 Other research has suggested that Malawi’s IMCI scale-up has made high-quality child health services more accessible to the population and that it saved 280,000 lives during this period, 60 percent of which were related to increases in iCCM, ITN use, and vaccinations.24
2. Formalizing HSAs as part of the salaried health workforce
For decades, Malawi has recognized the importance of community health providers in expanding health service coverage, responding to emergencies, and reaching hard-to-access populations. The country has slowly increased the number of HSA responsibilities over time, as shown in Figure 4 on page 6, and has also increased support to HSAs to help guarantee positive health outcomes.
Figure 4. Evolution of HSAs in Malawi 30-32
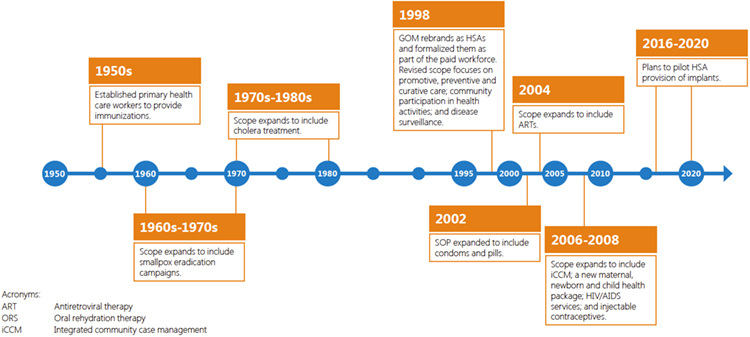
In 1998, the GOM made a strategic decision to formalize HSAs as part of the country’s health workforce and pay them salaries to support their effectiveness. A decade later, Malawi was still among a handful of countries in sub-Saharan Africa that paid community health providers a salary,25 which has become a practice of increasing popularity as countries have made efforts to standardize and bolster support to community health providers.26 Today, HSAs receive about US$63 per month, financed by the GOM through a pooled funding mechanism known as a Sector-Wide Approach.27 The institutionalization of HSAs has provided the country with a large and experienced community health workforce that is quick to mobilize to deliver key interventions.
One study showed that HSAs were satisfied with their status as salaried, government employees, citing it as a motivator and accountability mechanism.12 However, at the same time, some studies suggest that a number of setbacks common in resource-constrained settings threaten their motivation and performance. These include inconsistent payments, lack of a guaranteed pension plan, perceptions that salaries are too low, poor supervision, heavy workloads, no or unclear opportunities for refresher trainings and career advancement, and a desire for salary to be linked to merit rather than just position.12,28,29 Recent discussions in Malawi have indicated efforts to overcome some of these challenges,28 though some are pervasive workforce issues across many countries without simple solutions.
3. Engaging in public-private partnerships to improve access and quality
Established in the 1960s, the Christian Health Association of Malawi (CHAM) is the largest not-for-profit health provider in Malawi and has a strong presence in poor, rural, and remote communities. In 2015, CHAM owned 175 facilities, including 20 major hospitals, 30 community hospitals, 12 training institutions, and 113 health centers and provided care for 37 percent of Malawians.33 Historically, CHAM facilities charged user fees, constituting a barrier for many. Beginning in 2002, however, the GOM partnered with CHAM to create service-level agreements (SLAs) to help finance direct costs in CHAM facilities in exchange for removing user fees for EHP services.34 In 2015, 53 CHAM facilities were covered by SLAs.33
Studies have shown that this public-private partnership has increased coverage of health care services throughout the country, having helped clients overcome major financial and geographical barriers.33,35 A 2013 study showed that in one CHAM facility, the number of deliveries quadrupled between 2004 and 2010 while the number of child visits increased six-fold between 2008 and 2010.33 Furthermore, health providers and clients alike provided positive qualitative feedback about the SLA scheme.
Despite increased coverage, the GOM/CHAM partnership has encountered operational challenges, including lack of guidance outlining roles and responsibilities, standardizing reporting mechanisms, and aligning data collection and monitoring systems; reimbursement, billing, and payment issues; and increases in demand for services, which have left many CHAM facilities without necessary resources and forced them to revert to charging user fees for many EHP services.34-36
While the public-private partnership has expanded access, both parties must strengthen planning and management systems to meet the growing demands in health care and sustain gains. In 2016, the GOM and CHAM released operational guidelines to address some of these operational challenges.37
4. Using cStock to manage medical commodities in real time
A 2010 assessment of Malawi’s community health supply chain revealed poor data visibility, low HSA motivation, and transport as barriers to commodity availability.38 In 2011, the GOM and partner JSI Research & Training Institute, Inc. piloted an open-source web-based logistics management information system called cStock in six districts as part of a strategy to improve logistics reporting. cStock aimed to facilitate real-time reporting and management of supplies, which are of critical importance to HSAs, who may manage more than 19 types of commodities.39
cStock was designed specifically for the Malawian context, with input from relevant stakeholders at all levels of the health system. The system went through a series of iterations by supply chain experts and key users to improve usability and better meet local needs.
HSAs run cStock on their personal mobile phones to submit stock information and refill requests to health facilities. The program calculates resupply needs based on reported stock levels and system-calculated consumption. Additionally, a web-based dashboard provides real-time HSA commodity data and can produce customizable supply chain reports. Staff at the district and central levels can access the dashboard and thereby better monitor stock, identify problems, prioritize action, and respond.
As part of the cStock pilot, district product availability teams (DPATs) were established to ensure consistent product availability, improve data visibility, and bolster decision-making capacity. DPATs meet with facility staff and HSAs monthly to identify challenges related to stock management reporting and to develop plans to address them.
Through the cStock intervention, HSA reporting rates nearly doubled, averaging above 80 percent in all districts compared to 43 percent at baseline.39 In 2013, cStock was the primary means for HSAs to order health products, with 94 percent of HSAs in cStock districts using it and 92 percent of drug store in-charges using it to determine the quantities to resupply to HSAs.40 By mid-2014, the cStock pilot expanded to 24 districts, reaching over 2,500 HSAs, and the MOH and partners began planning for national scale-up, guided by a five-year transition plan to help the MOH manage the system independently.39
Figure 5. cStock Logistical Management Information System
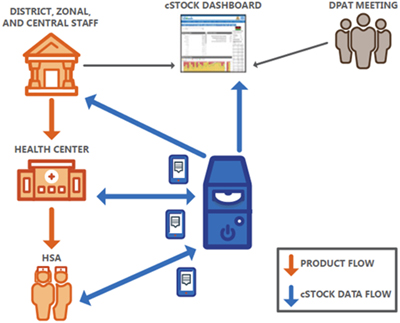
Overall, cStock provides HSAs and health facility staff with simple technology to request and resupply products, which eases reporting burdens, reduces staff travel time, helps flag low stocks and calculate resupply, and improves transparency and communication in the logistics system. Implementation challenges are largely infrastructural, such as poor network coverage, inconsistent access to electricity to charge phones, and connection problems.39
DPATs provided the cStock intervention a supportive, institutional structure to help ensure quality and longer term sustainability. Some of the reported benefits of the DPATs were that they enabled collective problem-solving, facilitated better performance, enabled knowledge sharing, allowed encouragement, and increased coordination and communication. Challenges included a lack of transportation, meeting length, low attendance, and poor district engagement and feedback.39
Lessons for Other Countries
In recent years, Malawi has used HSAs to expand access to basic health services and information within communities to improve health outcomes. The country has also adopted progressive strategies and scaled up innovative schemes that offer lessons for community health investments:
- Program “iteration” takes commitment and years of targeted investment. Malawi’s experience designing and scaling up community-based FP and iCCM demonstrates that a continuous and iterative process to develop, implement, evaluate, and adjust is an important ingredient for refining programs so that they achieve programmatic impact. For example, the country’s strong commitment to increasing contraceptive prevalence has resulted in receptivity to testing new and innovative FP methods and delivery approaches, most recently, the Sayana® Press pilot. Such initiatives have been built on a locally informed foundation of knowledge about what has worked over the past 25 years and on supportive policies that have evolved with the evidence.
- Build upon existing infrastructure and make refinements to scale interventions. Malawi was able to quickly scale iCCM by leveraging long-established HSAs, who had provided curative health services in communities since the 1990s. Furthermore, faced with the challenge of providing care to a large rural population—many of whom live in hard-to-reach areas—the country partnered with CHAM, which already had a vast network of health facilities throughout the country, to expand coverage. Countries scaling up interventions should consider existing infrastructure carefully and assess available resources to help ensure success.
- Service-level agreements between public and private sector can help expand coverage by leveraging respective resources. Appropriate administrative and operational structures must be put in place by the respective partners to ensure coordination, understanding of respective roles, and data sharing for sustained performance. The GOM/CHAM partnership may further benefit from standardized policy guidance; orientation on roles and responsibilities; and staff capacity-building on management and operational competencies, such as financial management and contract negotiation. Malawi’s experience also demonstrates that costing and modeling the impact of the partnership is crucial for planning, as CHAM’s facilities were overwhelmed by the increased volume of patients accessing their services.
- Engaging users in designing new tools and approaches and supporting continuous refinement can help reach desired outcomes by rapidly responding to changing needs. Malawi’s experience piloting and scaling up cStock illustrates that interventions designed specifically for the local context and involving users at various stages of product development can ensure use. cStock boosted data visibility and improved community health provider motivation, stock reporting, and performance. The cStock experience also demonstrated the importance of co-creating tools and systems with scalability and sustainability in mind from the outset.
- “Bread and butter” support to community health providers still matters. Although HSAs are formalized and salaried, evidence suggests that many lack critical mechanisms of support, such as refresher trainings, regular supervision, and timely payments. While a growing body of research documents the need for these inputs, their operationalization in many countries, including Malawi, often remains weak. Through the DPAT component of the cStock intervention, Malawi may have stumbled across a nontraditional but supportive institutional structure that helps HSAs problem-solve, share experiences, and ultimately improve the quality of their work. Exploring unconventional approaches to strengthen “bread and butter” program inputs, such as supervision and training, may reveal new opportunities to bolster and sustain community health provider performance. To this end, Malawi’s forthcoming National Community Health Strategy aims to strengthen HSA support systems through bolstering training, supervision, monitoring, and community engagement in health.41
Reference List
1 World Health Organization. 2015. Trends in Maternal Mortality 1990 to 2015: estimates by WHO, UNICEF, UNFPA, World Bank Group and the United States Population Division. Geneva: World Health Organization.
2 National Statistical Office [Malawi] and ORC Macro. 2001. Malawi Demographic and Health Survey 2000. Zomba, Malawi and Calverton, Maryland, USA: National Statistical Office and ORC Macro
3 National Statistical Office (NSO) [Malawi] and ICF International. 2016. Malawi Demographic and Health Survey 2015-16: Key Indicators Report. Zomba, Malawi, and Rockville, Maryland, USA. NSO and ICF International.
4 World Bank DataBank. 2016. “Mortality rate, under-5 (per 1,000 live births)” (accessed March 2017).
5 National Statistical Office (NSO) and ICF Macro. 2011. Malawi Demographic and Health Survey 2010. Zomba, Malawi, and Calverton, Maryland, USA: NSO and ICF Macro.
6 UNICEF. 2014. Committing to child survival: A promised renewed—Progress report 2014. New York, New York: UNICEF.
7 Smith, S., Deveridge, A., Berman, J., Negin, J., Mwambene, N., Chingaipe, E., … Martiniuk, A. (2014). Task-shifting and prioritization: a situational analysis examining the role and experiences of community health workers in Malawi. Human Resources for Health, 12, 24.
8 Callaghan-Koru, J. A., Hyder, A. A., George, A., Gilroy, K. E., Nsona, H., Mtimuni, A., & Bryce, J. (2012). Health Workers’ and Managers’ Perceptions of the Integrated Community Case Management Program for Childhood Illness in Malawi: The Importance of Expanding Access to Child Health Services. The American Journal of Tropical Medicine and Hygiene, 87(5 Suppl), 61–68.
9 Government of the Republic of Malawi. 2009. ![]() Health Surveillance Agent Training Manual Facilitator’s Guide (PDF, 1.7 MB). Lilongwe, Malawi: Ministry of Health.
Health Surveillance Agent Training Manual Facilitator’s Guide (PDF, 1.7 MB). Lilongwe, Malawi: Ministry of Health.
10 Ministry of Health (MoH) [Malawi] and ICF International. 2014. Malawi Service Provision Assessment (MSPA) 2013-14. Lilongwe, Malawi, and Rockville, Maryland, USA: MoH and ICF International.
11 Kristen Devlin, Kimberly Farnham Egan, and Tanvi Pandit-Rajani. 2016. Community Health Systems Catalog Country Profile: Malawi. Arlington, VA: Advancing Partners & Communities.
12 African Strategies for Health. 2015. ![]() Community Health Worker Incentives: Lessons Learned and Best Practices from Malawi. Arlington, VA: African Strategies for Health.
Community Health Worker Incentives: Lessons Learned and Best Practices from Malawi. Arlington, VA: African Strategies for Health.
13 Government of Malawi, Ministry of Health. 2016. District Health Information System Version 2 data (unpublished).
14 Chimbwete, C., Watkins, S. C., & Zulu, E. M. (2005). The Evolution of Population Policies in Kenya and Malawi. Population Research and Policy Review, 24(1), 85–106.
15 The ACQUIRE Project. 2005. ![]() Moving family planning programs forward: Learning from success in Zambia, Malawi, and Ghana. New York: The ACQUIRE Project/EngenderHealth.
Moving family planning programs forward: Learning from success in Zambia, Malawi, and Ghana. New York: The ACQUIRE Project/EngenderHealth.
16 National Statistical Office (NSO) [Malawi] and Macro International Inc. 1994. Malawi Demographic and Health Survey 1992. Zomba, Malawi, and Calverton, Maryland, USA: NSO and ICF International.
17 USAID. 2012. ![]() Three Successful Sub-Saharan Africa Family Planning Programs: Lessons for Meeting the MDGs. Washington, DC: USAID.
Three Successful Sub-Saharan Africa Family Planning Programs: Lessons for Meeting the MDGs. Washington, DC: USAID.
18 Advancing Partners & Communities. 2014. ![]() Provision of Injectable Contraceptives by Community Health Workers (PDF, 1 MB). Arlington, VA: Advancing Partners & Communities.
Provision of Injectable Contraceptives by Community Health Workers (PDF, 1 MB). Arlington, VA: Advancing Partners & Communities.
19 JSI Research & Training Institute, Inc. 2016. “Community-based Provision of Contraceptive Injectables: Home and Self Injection Study in Malawi” (accessed March 2017).
20 Government of Malawi. 2015. Malawi costed implementation plan for Family Planning, 2016-2020. Lilongwe, Malawi: Government of Malawi.
21 Rodríguez, D. C., Banda, H., & Namakhoma, I. (2015). Integrated community case management in Malawi: an analysis of innovation and institutional characteristics for policy adoption. Health Policy and Planning, 30(suppl_2), ii74-ii83.
22 Management Sciences for Health (MSH) and Management Solutions Consulting (MSC) Limited. 2010. ![]() Evaluation of Malawi’s Emergency Human Resources Programme. Cambridge, Massachusetts: MSH and MSC.
Evaluation of Malawi’s Emergency Human Resources Programme. Cambridge, Massachusetts: MSH and MSC.
23 Gilroy, K. E., Callaghan-Koru, J. A., Cardemil, C. V., Nsona, H., Amouzou, A., Mtimuni, A., … Bryce, J. (2013). Quality of sick child care delivered by Health Surveillance Assistants in Malawi. Health Policy and Planning, 28(6), 573–585.
24 Kanyuka, M., Ndawala, J., Mleme, T., Chisesa, L., Makwemba, M., Amouzou, A., … Colbourn, T. (2016). Malawi and Millennium Development Goal 4: a Countdown to 2015 country case study. The Lancet Global Health, 4(3), e201–e214.
25 George, A., Young, M., Nefdt, R., Basu, R., Sylla, M., Clarysse, G., … Diaz, T. (2012). Community Health Workers Providing Government Community Case Management for Child Survival in Sub-Saharan Africa: Who Are They and What Are They Expected to Do? The American Journal of Tropical Medicine and Hygiene, 87(5 Suppl), 85–91.
26 World Health Organization. 2015. Strengthening Primary Health Care through Community Health Workers: Investment Case and Financing Recommendations. Geneva, Switzerland: World Health Organization.
27 Jarrah, Z., Lee, A., Wright, K., Schulkers, K., and D. Collins. 2013. ![]() Costing of Integrated Case Management in Malawi. Arlington, VA: Management Sciences for Health.
Costing of Integrated Case Management in Malawi. Arlington, VA: Management Sciences for Health.
28 Kok, M. C., & Muula, A. S. (2013). Motivation and job satisfaction of Health Surveillance Assistants in Mwanza, Malawi: an explorative study. Malawi Medical Journal, 25(1), 5–11.
29 Chikaphupha, K. R., Kok, M. C., Nyirenda, L., Namakhoma, I., & Theobald, S. (2016). Motivation of health surveillance assistants in Malawi: A qualitative study. Malawi Medical Journal, 28(2), 37–42.
30 Nsona, H., Mtimuni, A., Daelmans, B., Callaghan-Koru, J. A., Gilroy, K., Mgalula, L., … Zamasiya, T. (2012). Scaling Up Integrated Community Case Management of Childhood Illness: Update from Malawi. The American Journal of Tropical Medicine and Hygiene, 87(5_Suppl), 54–60.
31 Katsulukuta, A. 2010. Improve Coverage: Opportunities and Challenges. Geneva: The Global Immunization Meeting.
32 Government of Malawi, Ministry of Health. 2012. The Health Surveillance Assistants: Origins and Current Status. Lilongwe, Malawi: Ministry of Health.
33 Christian Health Association of Malawi. 2015. ![]() 2015 Annual Report. Lilongwe, Malawi: Christian Health Association of Malawi.
2015 Annual Report. Lilongwe, Malawi: Christian Health Association of Malawi.
34 Chirwa, M. L., Kazanga, I., Faedo, G., & Thomas, S. (2013). Promoting universal financial protection: contracting faith-based health facilities to expand access - lessons learned from Malawi. Health Research Policy and Systems, 11, 27.
35 SHOPS Project. 2012. Malawi Private Health Sector Assessment. Brief. Bethesda, MD: SHOPS Project, Abt Associates
36 Tambulasi, R. (2014). When Public Services Contracts are Poorly Managed: An Analysis of Malawi’s Service Level Agreements. International Public Management Review, 15(1), 83–99.
37 Government of Malawi and Christian Health Association of Malawi. 2016. ![]() Service Level Agreement Guidelines. Lilongwe, Malawi: GOM and CHAM.
Service Level Agreement Guidelines. Lilongwe, Malawi: GOM and CHAM.
38 Shieshia, M., Noel, M., Andersson, S., Felling, B., Alva, S., Agarwal, S., … Chandani, Y. (2014). Strengthening community health supply chain performance through an integrated approach: Using mHealth technology and multilevel teams in Malawi. Journal of Global Health, 4(2).
39 SC4CCM Project. n.d. ![]() cStock: Deploying mHealth for improved product availability in Malawi. Arlington, VA: SC4CMM.
cStock: Deploying mHealth for improved product availability in Malawi. Arlington, VA: SC4CMM.
40 SC4CCM. 2013. Malawi Community Health Supply Chain Midline Assessment Report. Arlington, Va.: SC4CCM.
41 Government of the Republic of Malawi (forthcoming). National Community Health Strategy. Lilongwe, Malawi: Ministry of Health.
Recommended Citation
Kristen Devlin, Tanvi Pandit-Rajani, and Kimberly Farnham Egan. 2017. Malawi’s Community-based Health System Model: Structure, Strategies, and Learning. Arlington, VA: Advancing Partners & Communities.
