The Community-Based Health System Model Series briefs identify and discuss critical health system inputs and processes that have contributed to the implementation and expansion of communitybased service delivery in different countries. Countries were selected for their geographic diversity, type of service delivery model, and programmatic scale-up. This brief reviews Senegal’s community health model to inform future policy, program design, and implementation in other countries. Read briefs on Malawi | Nepal
Health Situation in Senegal

Photo IFPRI/Milo Mitchell
Since the 1990s, Senegal has made notable progress in key health indicators. Between 1990 and 2017, maternal mortality dropped from 540 to 236 deaths per 100,000 live births, and the percentage of fully vaccinated children steadily increased from 58.7 percent to 75 percent in approximately the same period.1-3 In just the past decade, child mortality more than halved from 121 to 56 deaths per live births, with a reduction in disparity between urban and rural households (Figure 1).3-4
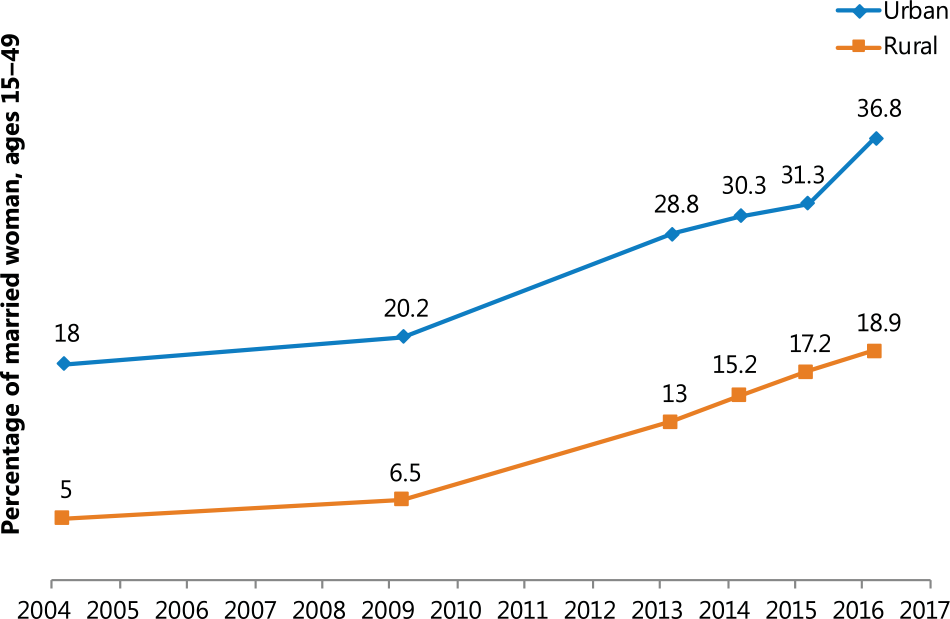
The country also made great strides in expanding access to modern family planning methods. Between 2005 and 2017, the percentage of married women using modern contraceptives more than doubled from 10.3 to 26.3 percent, and more than tripled among rural women from 5.0 to 18.9 percent (Figure 2). Unmet need for family planning declined from 30.1 to 21.9 percent.3-4 As a result, the total fertility rate has started to fall after years of stagnation; between 2014 and 2017, it declined from 5.0 to 4.6.3,5 Table 1 indicates key health data in Senegal.
Table 1. Current Health Statistics in Senegala
| Total populationb | 16.3 m |
| Rural populationb | 54% |
| Total fertility rate | 4.6 |
| Contraceptive prevalence rate (modern methods) | 26.3% |
| Unmet need for contraception | 21.9% |
| Maternal mortality ratio (per 100,000 live births) | 236 |
| Neonatal mortality rate (per 1,000 live births) | 28 |
| Infant mortality rate (per 1,000 live births) | 42 |
| Under-five mortality rate (per 1,000 live births) | 56 |
| Percentage of births delivered by a skilled provider | 68.4% |
| Percentage of children under 5 years moderately or severely stunted | 16.5% |
| Percentage of households with an improved source of drinking water | 81.0% |
| Percentage of women reporting distance to a health facility as a problem in accessing care | 22.1% |
| Adult HIV prevalencec | 0.4% |
| Total expenditure on health per capita (current US$)d | $36 |
a Data is from the Senegal Demographic and Health Survey, 2017 (continuous), unless otherwise noted.
b Population Reference Bureau (PRB). 2018. 2018 World Population Data Sheet. Washington, DC: PRB.
c UNAIDS. 2015. “HIV and AIDS estimates” (2017).
d World Bank Data Bank 2010-2015. “Health expenditure per capita (current US$).”
Senegal’s investments to target health education and services to underserved areas contributed to these improvements. The country prioritized community health and promoted coordination among health and development partners. It also invested in strategies to pilot and scale up key community-based interventions, strengthen supply chains, and engage community members to promote healthy practices, strengthen service delivery, and advocate for their own health. However, to reach targets such as the Sustainable Development Goals, Family Planning 2020 commitments, and universal health coverage (UHC), Senegal must continue to adapt and build upon its approaches to advance the health of its population.
Figure 1. Under-five Mortality, 2005–2017
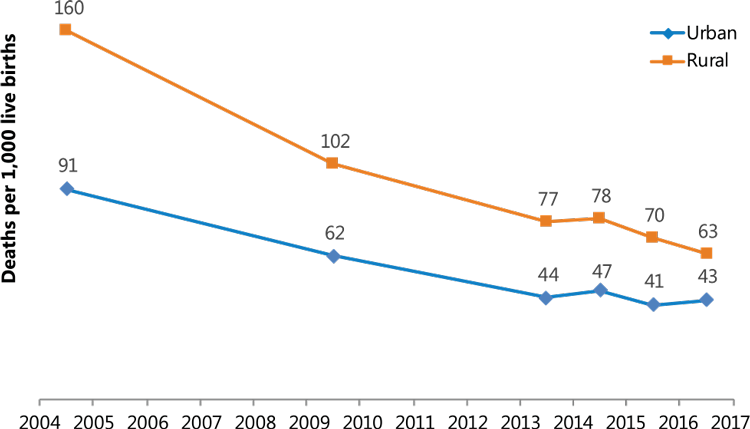
Figure 2. Modern Contraceptive Use in Married Women, 2005–2017
Senegal’s Health System Structure: Expanding Access to Underserved Communities
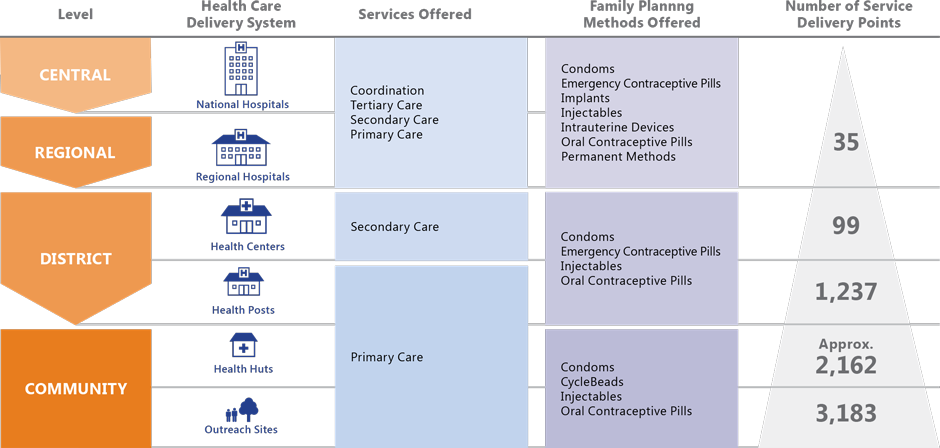
Senegal’s large rural population, poor infrastructure, arid climate, and long distances between communities and health facilities have historically impeded people’s ability to access services. In the mid1990s, the government decentralized the health system so that district and community authorities could plan and roll out context-specific approaches to improve service delivery. Today, each of the country’s 76 health districts has at least one health center and several health posts, and a network of community-based health huts and outreach sites to extend services to communities that otherwise would not have access to them. Community health providers offer health information, education, and services from the health huts and outreach sites.
The Ministry of Health and Social Action (MSAS) sets the community health agenda, provides programmatic oversight, and develops strategic and policy guidance. In 2009, MSAS launched the National Health Development Plan as a framework to achieve UHC, which emphasizes scaling up key health interventions in partnership with communities.6 In 2014, Senegal produced its first national community health strategy to strengthen subnational decision-making; foster community ownership to address health inequity; harmonize programs and service packages; improve community health provider motivation; strengthen governance and supply systems; and move toward sustainable health systems.7
Several large-scale programs supported by the United States Agency for International Development (USAID) and other development partners in the past decade have also contributed to Senegal’s progress. Table 2 summarizes the achievements of three recent programs.
Table 2. Selected Achievements of Large-scale USAID-funded Community Health Programs in Senegal, 2006–20218-10
| YEARS | PROJECT NAME | ACHIEVEMENTS |
|---|---|---|
| 2006–2011 | Community Health Program (CHP) I |
|
| 2011–2016 | CHP II |
|
| 2016–2021 | Integrated Service Delivery and Health Behaviors project |
|
Figure 3 on page 4 provides an overview of Senegal’s health system structure and illustrates the type of services available at each level, using family planning as an example.
Community Health Providers: Policy to Service Delivery
Senegal’s five main community health provider cadres provide specific interventions as part of an integrated package of health services: agents de santé communautaires (ASCs); matrones; bajenu gox; home-based care providers (DSDOMs); and relais communautaires (relais). Table 3 outlines their scopes of practice and other components of Senegal’s community health system.
Table 3. Senegal’s Community Health Providers7,11,15
| Supportive policy |
|
| Scope of practice |
|
| Supervision and management | Staff from health posts, district health offices, and nongovernmental organizations (NGOs) supervise community health providers on a bimonthly basis using standardized, integrated tools. |
| Commodities and Community health providers access commodities and education materials from health huts and health posts. Certain cadres provide materials | Community health providers access commodities and education materials from health huts and health posts. Certain cadres provide commodities for iCCM, such as antibiotics for acute respiratory infections; artemisinin combination therapy for malaria; and oral rehydration salts and zinc for diarrhea. Some offer CycleBeads, condoms, oral contraceptive pills, and injectable contraceptives. Matrones administer medicines for postpartum hemorrhage. Health post in-charges restock health huts as needed. |
| Training | Training curricula are standardized and include refresher trainings but vary by cadre. |
| Renumeration* | Renumeration is determined at the local level and may include cash payments; allowances financed through user fees and cost-recovery systems; performance-based payments; small profits from commodity sales; community committee memberships; badges; certificates; commemoration days; and tickets for pilgrimages to holy sites. |
| Referrals | Bajenu gox, relais, and DSDOMs refer clients to ASCs and matrones for services not within their scope. ASCs and matrones may refer clients to health posts, and health post staff counter-refer clients for follow-up. |
| Health promotion | All providers conduct health promotion in collaboration with community groups and committees. |
| Monitoring and reporting | Community health providers complete monthly reports and submit them to health post staff, who then input aggregate data into the health management information system. Providers and community members review data to inform decision-making. |
*Remuneration, such as cash and performance-based payments, is not used to incentivize family planning care.
Key Strategies for Strengthening and Scaling Up Community Health in Senegal
1. Revitalizing a network of community-based health huts under a unified yet flexible strategy
People in rural Senegal have accessed health services from health huts since the 1950s,15 but for years, there was no concerted, harmonized approach for the government and partners to support health hut operations. In 2006, USAID launched the Community Health Program (CHP), which revitalized, expanded, and coordinated the health hut system to extend coverage of a package of basic health services and improve primary health care. The MSAS provided oversight to the CHP, and a consortium of NGOs led by ChildFund International implemented the program in nearly all regions of the country.
Figure 3. Senegal’s Public Health System11-14
Under the health hut system, one ASC and one matrone provide basic services from each hut, and other community health providers, such as relais, conduct outreach. The head nurse from a neighboring health post supervises and receives referrals from the providers. The CHP NGOs also recruit and train community development agents to supervise community health providers, monitor activities, and facilitate reporting. Ideally, community members themselves help construct and manage the huts.
Although unified by an overarching approach, each CHP NGO developed unique strategies to support health huts in their respective areas to meet local needs. For example, CHP NGOs designed different ways to engage communities in health hut management. This flexibility allowed the program to reduce costs and improve effectiveness by using resources and networks in their respective catchment areas.16 To internally align their work, the NGOs held quarterly meetings to compare indicators, discuss problems, provide updates, and showcase their approaches during field visits. They also held regular consultations and joint supervision visits with the MSAS.17
Between 2006 and 2011, the CHP transformed health huts from under-resourced, understaffed, and sometimes completely nonfunctional structures to a network of 1,620 facilities in 13 regions that provided integrated, community-based services. The partnership supported scale-up, coordination, and standardization in data systems, as well as training, staffing, and reporting across regions. In 2011, most huts offered a full service package, which led to improvements in utilization of services. Health post staff reported a 20–30 percent reduction in caseload due to task shifting certain services (e.g., provision of oral contraceptive pills and treatment of simple cases of diarrhea and respiratory infections) to community health providers.17
These successes prompted the second iteration of the CHP, implemented between 2012 and 2016, which expanded the health service package and increased the number of health huts and outreach sites. Today, as many as 2,162 health huts and 3,183 outreach sites operate across the country, connecting 70 percent of Senegal’s nine million people with the formal health system.18
However, the question of how to sustain the health hut system has plagued the MSAS and partners since the beginning of the first CHP. Health huts remain dependent on partners, and though communities help sustain facilities (e.g., by constructing new huts, subsidizing drugs, and collecting financial payments for providers),19,20 they have been most successful where NGO backstopping is strong.17 Additional barriers include insufficient community awareness, frequent stockouts, inconsistent service quality, and low provider motivation, lack of recognition, and limited opportunities for professional growth.9
Nevertheless, the health hut network created the foundation of a functional community health system. In 2014, Senegal recognized health huts as part of the formal health system and committed to further investments as part of its first national community health strategy. The country will need to identify financing models to help sustain and build upon these achievements.
2. Generating and using evidence to improve reproductive, maternal, newborn, and child health
Senegal has long recognized that reaching women and children in remote communities with basic health interventions is essential to achieving health objectives, and is a leader in testing and institutionalizing community-based innovations.
Senegal was among the first African countries to pilot and nationally scale iCCM. Historically, the role of Senegal’s community health providers was limited to disease-prevention education and provision of basic treatment, such as oral rehydration therapy for diarrhea and chloroquine for malaria. Encouraged by a 2003 study in Nepal on community-based treatment of pneumonia, a committee of national leaders, researchers, and advocates in Senegal conducted a feasibility study which determined that community health providers were capable of treating acute respiratory illnesses with antibiotics. In 2005, the MSAS integrated the intervention into the package of services offered at health huts, demonstrating commitment to applying experience and scientific research to change policy and practice.19
Over the next few years, the country piloted other interventions related to iCCM: treating malaria with artemisinin combination therapy, adding zinc to diarrhea management protocols, and diagnosing malaria with rapid diagnostic tests before treating, which reduced the number of children who unnecessarily received malaria medications.21-22 Instead of introducing all interventions simultaneously, Senegal added them gradually, which facilitated scale-up by allowing more time to train community health providers. Figure 4 outlines the evolution of community health services in the country.
Figure 4. Evolution of Senegal’s Community-Level Health Services15
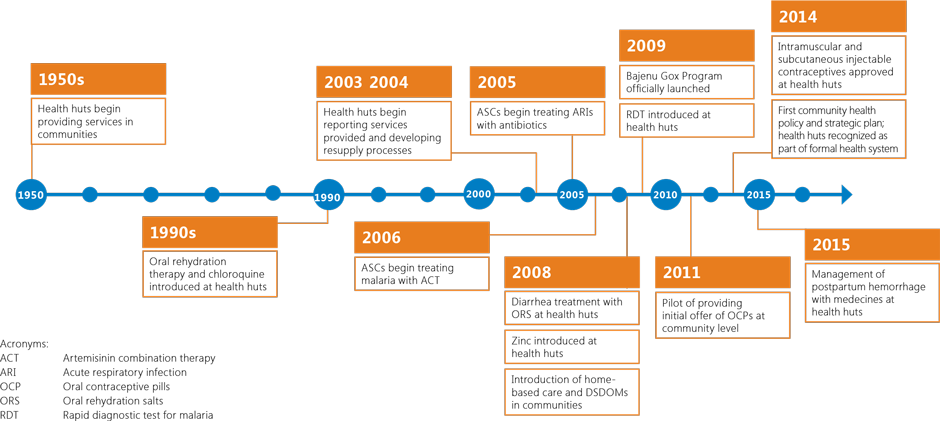
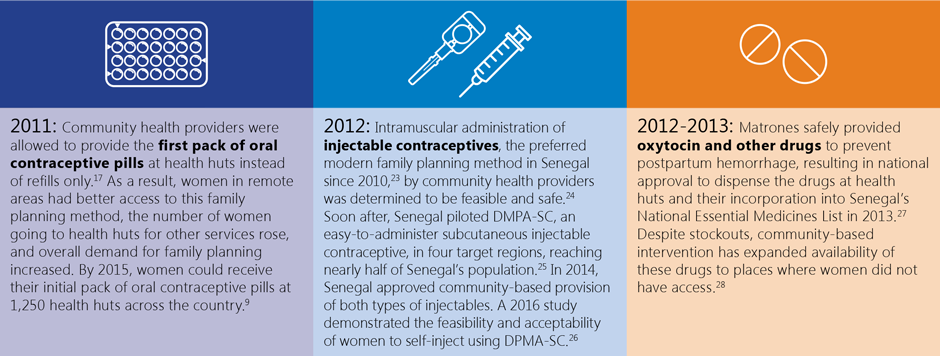
Senegal adopted a similar, gradual approach when it expanded the DSDOM scope of work. In 2008, the country allowed these providers to test for and treat simple malaria cases. Because of their effectiveness, the MSAS trained the DSDOMs to provide additional iCCM interventions in 2013. Figure 5 showcases other key community-based interventions the country has piloted and scaled.
Figure 5. Community-based RMNCH Pilots
Senegal’s focus on testing new community-based interventions exemplifies its commitment to broadening access to a wide array of services for RMNCH, including newer contraceptive technologies. However, program implementation and scale-up have encountered common health system roadblocks including delays in staff training; intermittent product availability; and low service uptake due to insufficient knowledge of danger signs among caregivers, community-provider mistrust, inability to pay for services, and subpar service quality.29-32
3. Engaging and training bajenu gox to promote healthy behaviors, support providers, and advocate for health

Photo: Akua Kwateng-Addo/USAID
Senegal launched the bajenu gox program in 2009 to reduce maternal and child morbidity and mortality. “Bajenu gox” roughly translates as “godmothers” and refers to respected female elders who are active members of their communities and advocate for the well-being of women, girls, and families. Traditionally, bajenu gox counsel younger women on topics like marriage, pregnancy, delivery, and health. The bajenu gox program formalized these women into volunteer health promoters because of their ability to influence fellow community members’ behavior.
Bajenu gox promote RMNCH interventions such as antenatal care, voluntary family planning, and child vaccination. They also mobilize communities, make home visits and referrals, and support other health activities. While the country developed a national bajenu gox curriculum in 2010, the MSAS and partners have also trained them to conduct activities in response to emerging national priorities. For instance, in 2013, one NGO trained 90 bajenu gox to educate their communities on gender issues, family planning, and HIV testing,33 and during the West Africa Ebola outbreak in 2015, 300 of them learned how to lead community conversations on preventing Ebola and other communicable diseases.34
By 2015, 3,406 bajenu gox served communities across Senegal. Bajenu gox believe they have been instrumental in improving the health of their communities, particularly by helping women trust ASCs and other providers.12,18 A study found that bajenu gox improved outreach, particularly for family planning, to men and mothers-in-law, who are critical to household decision-making.31 In 2014, a group of bajenu gox were trained to develop advocacy strategies to mobilize local funds for family planning commodities. In one case, bajenu gox convinced the mayor to allocate funds from a communal budget for family planning, demonstrating that with the appropriate support, bajenu gox can be effective advocates.35
Despite these accomplishments, the bajenu gox program faces low retention and motivation due to poor supervision and monitoring, limited remuneration, and insufficient integration with other community actors and initiatives.12,31 In response, the MSAS and partners plan to use a $3.6 million USAID investment to revitalize the bajenu gox program. Funds will be used to recruit additional bajenu gox and build their capacity for family planning promotion, improve supervision, and organize bajenu gox support networks.7 The MSAS also plans to give bajenu gox badges and bags, organize special events to recognize their work, and harmonize motivation schemes across the country.
4. Committing to community-level strategies
Across different health areas, Senegal has matched commitments with investments in community-level approaches. Recent advances in family planning illustrate the power of national leadership and follow-through, with special attention to the local level.
Although many initiatives have contributed to the recent rapid rise in modern contraceptive use, the 2011 Ouagadougou Conference on Family Planning and the 2012 London Summit on Family Planning ignited a particularly organized and focused effort to prioritize voluntary family planning as a health and development issue. Following the Summit, the president, prime minister, and other high-level officials elevated the visibility and importance of family planning for the country. The MSAS established a Directorate for Reproductive Health and Child Health, and developed the 2012–2015 National Action Plan for Family Planning. Senegal also tripled its budget line for contraceptive products in 2012, and launched a technical family planning steering committee to convene stakeholders to discuss technical and financial concerns and enhance coordination. As a result, parliamentarians, other development sectors, NGOs, civil society, and financial partners are more engaged in family planning issues because they perceived it as a more organized discipline with a clearer vision.31
The 2012–2015 National Action Plan prioritized community-based family planning and community mobilization as necessary components to increasing overall family planning uptake.36 Communication campaigns and targeted messaging improved community acceptance and participation in family planning interventions, especially by men and religious leaders.31 Health staff increased outreach in communities, adding 12,962 new family planning users between 2012 and 2014.37 Shifting provision of oral contraceptive pills and injectable contraceptives to community health providers increased the accessibility of these methods, especially for rural women.38
The country’s 2016–2018 Strategic Framework for Family Planning outlines plans to allocate one-fifth of the family planning budget to community-level strategies, including adding 840 new health huts; rehabilitating and equipping current huts; recruiting new community health providers; and continuing to build community health provider capacity, including training DSDOMs to deliver certain family planning methods.39 Such investments will not only advance family planning but also help strengthen overall community-level service delivery.
Figure 6. The Informed Push Model and Previous ‘Pull’ System.
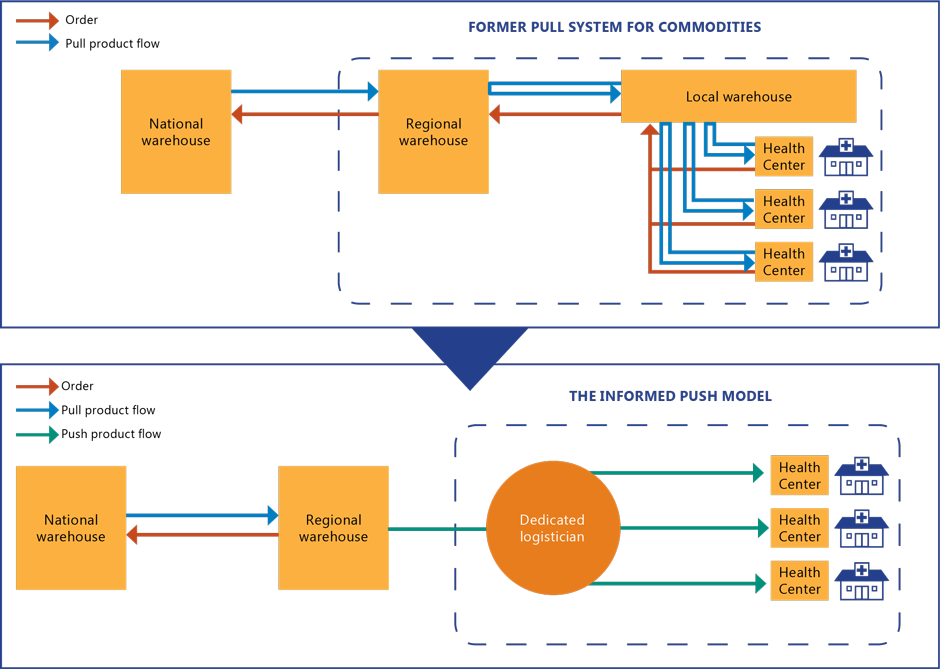
This figure was adapted from the IPM figure in Daff et al. 2014 (see reference 40).
5. Implementing an “Informed Push Model” to reduce contraceptive stockouts

Photo: Dominic Chavez/The Global Financing Facility
In 2011, the MSAS and its partners introduced the Informed Push Model (IPM) to reduce family planning commodity stockouts in health facilities. Under the IPM, a professional logistician collects family planning commodities from regional supply pharmacies on a regular basis, stores the products, and distributes them to district-level health facilities and pharmacies. Senegal modeled the IPM after a similar approach in Zimbabwe, and implemented it through a public-private partnership. Previously, the country had utilized a “pull’ model, in which health facility staff tracked and forecasted inventory and ordered commodities as needed.
The IPM sought to reduce the logistical burden on service providers by delivering supplies before they ran out. The logistician travels to health facilities to take inventory, record consumption data, and complete delivery slips and stock inventory reports. A software application called Comtrack tracks the process and allows regional logistics managers to monitor data across facilities and pharmacies to inform forecasting. The data also helps assess the functionality of the national family planning program.40 Figure 6 illustrates the IPM.
Under the IPM, facilities pay only for the products sold, as opposed to the previous pull system, in which they paid at the time of order, which caused problems when funds were insufficient. The IPM reinvests money collected from client user fees into restocking Photo: Dominic Chavez/The Global Financing Facility contraceptives and contracting logisticians. Furthermore, delivery teams bring commodities directly to facilities rather than requiring facility staff to pick up commodities during their workday and at their own expense.
A six-month IPM pilot eliminated stockouts of implants and injectable contraceptives, a reduction from 83 and 43 percent, respectively.40 At the end of one year, contraceptive uptake skyrocketed, increasing 127 percent for pills; 121 percent for injectables; 2,081 percent for implants; and 68 percent for IUDs,i corresponding to an estimated equivalent of an 11 percent point increase in modern contraceptive prevalence. The availability of a full range of contraceptive methods enabled health workers to counsel clients more effectively, and clients left facilities with their preferred family planning method, decreasing the likelihood of discontinuation. Health workers were also able to spend more time delivering family planning and other services instead of managing supplies.
i Reflects the average monthly consumption of contraceptives in 140 public health facilities in the Dakar region between February 2012 and March 2013. Pills increased from 1,544 to 3,503; injectables from 992 to 2,190; implants from 16 to 349; and IUDs from 34 to 57.
By 2015, Senegal had expanded the IPM to 1,375 sites in all 14 regions of the country, and stockout rates hovered around only two percent.41 Likewise, contraceptive uptake surged during IPM scale-up.42 In 2015, Senegal received the Resolve Award at the World Health Assembly for making headway toward universal access to reproductive health services.43
Although the IPM’s impact at the community level is not immediately apparent, in August 2016, Senegal launched an expanded IPM model called Yeksi-naa, which seeks to improve access to an array of essential medicines (e.g., for RMNCH, malaria, HIV, and tuberculosis) at all service delivery points, including health huts, for all citizens regardless of income or location. By October 2017, the country had trained approximately 2,900 health workers in stock management and pharmacovigilance; established a performance management system to enhance facility data collection and use; and introduced 40 new products into the IPM.44 As of 2018, the model distributed 90 essential health products to facilities around the country.42
Lessons for Other Countries
In just the past few years, Senegal has demonstrated how committed national leadership, investments in new and promising health interventions and service delivery models, and efforts to engage communities as partners can improve health for all. Senegal’s story offers key lessons to other countries seeking to strengthen community health systems:
- Harmonizing interventions across community health partners, while providing some flexibility to locally adapt them, enhances implementation effectiveness. As part of the CHP I and II, the MSAS and partners devised an overarching approach to guide NGOs to strengthen and scale up delivery of a package of community-based interventions. NGOs were successful in part because each was familiar with the unique needs, actors, and resources available in its area of intervention and had some latitude to tailor approaches accordingly. However, countries should consider and prepare for the challenges in coordinating multiple partners to ensure high-quality, equitable implementation.
- “Collaboration, learning, and adaptation” builds evidence to strengthen scale-up. Together, the MSAS, NGO partners, and local-level actors collaborated to advance the learning agenda for community health, including pioneering studies that demonstrated that community health providers could administer certain RMNCH interventions that they had not been able to provide previously. Gradually scaling each intervention allowed sufficient time to monitor and adapt implementation to available resources and the local context without overwhelming community health providers with too many new tasks. Similarly, the incremental extension of the health hut system over several years permitted the MSAS and partners to assess performance, identify lessons, and adapt strategies to subsequent iterations of programming. Finally, the country applied this “collaborating, learning, and adaptation” approach in demonstrating the effectiveness of the IPM in reducing stockouts, and building upon that foundation to scale up the model and add commodities under Yeksi-Naa.
- Formalizing community engagement approaches supports local ownership of health services. For years, health huts exemplified community engagement in health. Senegal’s decision to systematize and scale up this concept in the 2000s resulted in a network through which it could strengthen service delivery, reach more people, and institutionalize the community’s role in health. Senegal’s inclusion of health huts as formal MSAS structures in 2014 reiterated their importance and solidified the community engagement concept. At the same time, the country formalized the roles of trusted community members, such as bajenu gox, and systematically supported them to become community health promoters, mobilizers, and advocates.
- You get what you give: The community health workforce needs sufficient and sustainable motivation schemes to ensure quality and retention. With five community health provider cadres, Senegal’s community health programs rely heavily on the performance of its health workforce, but low staff motivation contributes to high turnover, poor service quality, and negative interactions with patients. To improve support for community health providers, recent strategies have allocated more funding for training, supervision, and equipment. Additionally, Senegal’s overarching community health strategy presents various financial and nonfinancial motivation schemes. Such investments are essential for ensuring community health providers are motivated and equipped to carry out high-quality work.
- Designing for sustainability at inception is paramount. Partnerships between the MSAS and health and development entities have yielded promising health outcomes, but dependence on foreign aid threatens sustainability. Having acknowledged this challenge for many years, the MSAS and partners consistently included strategies and made investments to support local ownership of health service delivery. The latest USAID-supported community health program in Senegal, the Integrated Service Delivery and Health Behaviors project, incorporates sustainability strategies into its design, informed by lessons from CHP I and II. This project’s scope is confined to certain areas of the country, permitting a greater focus on quality improvement. Its health systems strengthening approach supports self-reliance by building the capacity of individuals from the local to national level, and strengthening and aligning behavior change communication initiatives to increase individual and local community engagement in health governance and financing.
Reference List
6 World Health Organization. 2015. Trends in Maternal Mortality 1990 to 2015: estimates by WHO, UNICEF, UNFPA, World Bank Group and the United States Population Division. Geneva: World Health Organization.
7 Division des Statistiques Démographiques, Direction de la Prévision et de la Statistique, Ministère de l’Economie, des Finances et du Plan [Sénégal], and Macro International. 1994. Enquête Démographique et de Santé au Sénégal (EDS-II) 1992/93. Calverton, Maryland: Macro International.
8 Agence Nationale de la Statistique et de la Démographie (ANSD) [Sénégal], and ICF. 2018. Sénégal: Enquête Démographique et de Santé Continue (EDS-Continue 2017). Rockville, Maryland, USA: ANSD and ICF.
9 Ndiaye, Salif, et Mohamed Ayad. 2006. Enquête Démographique et de Santé au Sénégal 2005. Calverton, Maryland, USA: Centre de Recherche pour le Développement Humain [Sénégal] and ORC Macro.
10 Agence Nationale de la Statistique et de la Démographie (ANSD) [Sénégal], et ICF. 2016. Sénégal : Enquête Démographique et de Santé Continue (EDS-Continue 2015). Rockville, Maryland, USA : ANSD et ICF.
11 Ministry of Health and Prevention. 2009. Plan National de Développement Sanitaire (PNDS) (2009–2018).
12 Community Health Unit, Directorate General of Health, Ministry of Health and Social Action. 2014. Plan Stratégique de Santé Communautaire 2014–2018.
13 Ministry of Health and Social Action, National Coordination Unit. N.d. Programme Santé USAID/Santé Communautaire Phase 11 2011-2016. ChildFund Senegal.
14 MEASURE Evaluation. 2015. Health Service Integration: A Case Study. MEASURE Evaluation: Chapel Hill, NC.
15 USAID. 2015. “USAID/Senegal Health Project 2016-2021: Redacted Project Appraisal Document (PAD).”
16 Devlin, Kristen, Kimberly Farnham Egan, and Tanvi Pandit-Rajani. 2016. Community Health Systems Catalog Country Profile: Senegal. Arlington, VA: Advancing Partners & Communities.
17 Ernst & Young LLP. 2015. USAID/Senegal Final Mid-Term Evaluation Report. Contract No.: AID-685-C-14-00001.
18 Tine, Justin, Sophie Faye, Sharon Nakhimovsky, and Laurel Hatt. 2014. Universal Health Coverage Measurement in a Lower-Middle-Income Context: A Senegalese Case Study. Bethesda, MD: Health Finance & Governance Project, Abt Associates Inc.
19 National Program for the Fight against Malaria, Ministry of Health and Social Action. 2015. Plan Stratégique National de Lutte Contre le Paludisme au Sénégal 2016-2020.
20 Jarrah, Z., K. Wright, C. Suraratdecha, and D. Collins. 2013. Costing of Integrated Community Case Management in Senegal. Arlington, VA: Management Sciences for Health.
21 Story, William T., Karen LeBan, Laura C. Altobelli, Bette Gebrian, Jahangir Hossain, Judy Lewis, Melanie Morrow, et al. 2017. “Institutionalizing Community-Focused Maternal, Newborn, and Child Health Strategies to Strengthen Health Systems: A New Framework for the Sustainable Development Goal Era.” Globalization and Health 13 (June).
22 Barry, S., Putnam, E. Touré, C. 2011. Lessons learned from the USAID/Sénégal Community Health Program (CHP). Boston, MA: Initiatives, Inc.
23 ChildFund. 2016. “The Message of Health in Senegal.” Accessed August 19, 2019.
24 Maternal and Child Health Integrated Program (MCHIP). 2012. Integrated Community Case Management of Childhood Illness: Documentation of Best Practices and Bottlenecks to Program Implementation in Senegal. Washington, DC: MCHIP Jhpiego.
25 Tall, Alioune Badara, Pape Gallo Sow, Abdoul Aziz Ndiaye, and Ousseynou Ka. 2015. “Perception of Beneficiaries and Stakeholders about the Services Offered by Health Huts Put in Place by the Health Project—Community Health of USAID in the Goudomp Health District (Senegal).” Health 07: 1075.
26 Starbuck, Eric, Serge Raharison, Kerry Ross, and Dyness Kasungami. 2013. Integrated Community Case Management: Findings from Senegal, the Democratic Republic of the Congo, and Malawi A Synthesis Report. Washington, DC: Maternal and Child Health Integration Program.
27 Programme Nationale de Lutte contre le Paludisme. 2009. La Prise en Charge des Cas de Paludisme à Domicile au Sénégal: Leçons Apprises. Accessed October 2018.
28 Agence Nationale de la Statistique et de la Démographie (ANSD) [Sénégal], and ICF International. 2012. Enquête Démographique et de Santé à Indicateurs Multiples au Sénégal (EDS-MICS) 2010-2011. Calverton, Maryland, USA: ANSD and ICF International.
29 FHI 360. 2013. Senegal: Community Health Workers Successfully Provide Intramuscular Injectable Contraception. Research Triangle Park, NC: FHI 360.
30 Intrahealth International. 2015. Senegal Country Brief. Chapel Hill, NC: Intrahealth International.
31 Cover, Jane, Maymouna Ba, Jeanette Lim, Jennifer Kidwell Drake, and Bocar M. Daff. 2017. “Evaluating the Feasibility and Acceptability of Self-Injection of Subcutaneous Depot Medroxyprogesterone Acetate (DMPA) in Senegal: A Prospective Cohort Study.” Contraception 96 (3): 203–10.
32 Rashid, Shafia. 2017. “Misoprostol for Postpartum Hemorrhage: Empowering Health Workers to Save Lives.” Maternal Health Task Force (blog). January 5, 2017.
33 Gynuity Health Projects. N.d. From Research to National Scale-Up: Expanding Uterotonic Coverage for Postpartum Hemorrhage Prevention in Rural Senegal. New York, NY: Gynuity Health Projects.
34 Agence Nationale de la Statistique et de la Démographie (ANSD) [Sénégal] and ICF International. 2012. Enquête Continue sur la Prestation des Services de Soins de Santé (ECPSS) du Sénégal 2012-2013. Calverton, Maryland, USA: ANSD and ICF International.
35 Ministry of Health and Social Action, Directorate of Reproductive Health and Child Survival. 2016. Cadre Stratégique National de Planification Familiale 2016-2020.
36 Mbow, Fatou Bintou, Leslie Dubent, Nafissatou Diop, Fatou Ndiaye, Bocar Mamadou Daff, and Babacare Mané. 2017. Assessment of the implementation and achievements of the 3D Approach within the National Family Planning Action Plan (NFPAP) in Senegal – Summary Report. Dakar, Senegal: Population Council, The Evidence Project.
37 African Strategies for Health (ASH) project. 2016. Demand-Side Determinants to Integrated Community Case Management Care-Seeking. Arlington, VA: Management Sciences for Health, ASH project.
38 Ministry of Women, Children, and Female Entrepreneurship, Directorate of Gender Equity and Equality and Directorate of the Family. 2013. “Rapport de formation des “Bajenu Gox” en genre, santé de la reproduction / planification familiale et dépistage du VIH.” Dakar, Senegal: Ministry of Women, Children and Female Entrepreneurship.
39 Save the Children. 2015. “Formation de 300 Bajenu Gox et de 116 Maejt sur la prévention de la MVE.” Accessed August 15, 2017.
40 Advancing Family Planning. 2015. Mobilizing Mayoral Support in Senegal. Baltimore, MD: Advance Family Planning, Bill & Melinda Gates Institute for Population and Reproductive Health, Johns Hopkins Bloomberg School of Public Health.
41 Health Policy Project. 2013. Repositioning Family Planning in Senegal: Status of Family Planning Programs in Senegal. Washington, DC: Futures Group.
42 [No author]. N.d. Midterm Evaluation of the Plan d’Action National de Planification Familiale (draft).
43 Fleischman, Janet and Cathryn Streifel. 2016. Accelerating momentum the Momentum: U.S. Support for Women’s and Family Health in Senegal. Washington, DC: Center for Strategic and International Studies.
44 Ministry of Health and Social Action, Directorate of Reproductive Health and Child Survival. 2016. Cadre Stratégique National de Planification Familiale 2016-2020.
45 Daff, Bocar Mamadou, Cheikh Seck, Hassan Belkhayat, and Perri Sutton. 2014. “Informed Push Distribution of Contraceptives in Senegal Reduces Stockouts and Improves Quality of Family Planning Services.” Global Health: Science and Practice 2 (2): 245–52.
46 Ndiaye Ndao, Oumy Kalsoum. 2016. “Informed Push Model and the Last Mile: Integrating Other Health Products to the IPM Approach in Senegal.” Presented at the General Membership Meeting of the Reproductive Health Supplies Coalition, Seattle, Washington, October 14.
47 English, Allyson, Chloe Lanzara, Arunima Awale, and Laurel Hatt. 2018. Measuring What Matters: Case Studies on Data Innovations for Strengthening Primary Health Care. Washington, DC: Primary Health Care Performance Initiative.
48 Intrahealth International. 2015. “Senegal Wins 2015 Resolve Award for Informed Push Model of Contraceptive Distribution.” Accessed December 12, 2018.
49 Intrahealth International. 2017. Senegal Country Brief. Chapel Hill, NC: Intrahealth International.
Recommended Citation
Kristen Devlin, Tanvi Pandit-Rajani, and Kimberly Farnham Egan.” 2019. Senegal’s Community-based Health System Model: Structures, Strategies, and Learning. Arlington, VA: Advancing Partners & Communities.
APC would like to acknowledge Lamine Thiam, Senior Health Systems Strengthening and Program Management Expert, for his contributions in reviewing this brief.
